Cell子刊:小分子组合疗法促进心脏再生,或可治疗心梗!
2022-08-18 北京大学化学与分子工程学院 北京大学化学与分子工程学院
首次报道了5个小分子药物组合可以有效促进成年大鼠心脏再生,并且证明该药物组合对心肌梗塞有良好的治疗作用。
2022年4月7日,北京大学化学与分子工程学院、北大-清华生命科学联合中心雷晓光教授团队与北京大学未来技术学院熊敬维教授以及复旦大学赵世民教授团队合作在Cell Stem Cell杂志上发表了题为 A small molecule cocktail promotes mammalian cardiomyocyte proliferation and heart regeneration 的科研论文, 首次报道了5个小分子药物组合可以有效促进成年大鼠心脏再生,并且证明该药物组合对心肌梗塞有良好的治疗作用。
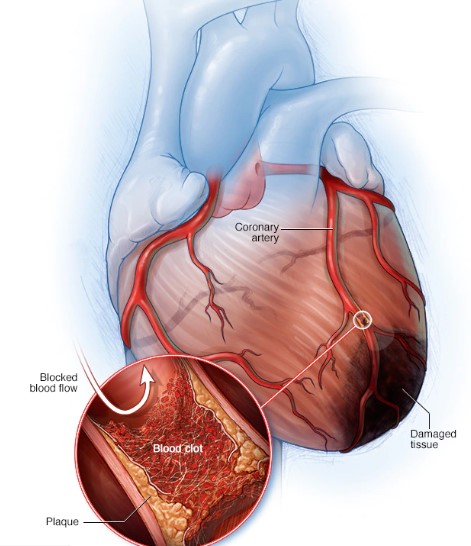
心血管疾病是威胁人类健康的头号杀手,其中急性心梗可导致心肌细胞大量死亡,而剩余的心肌再生能力有限,最终导致心脏纤维化和心力衰竭。目前临床上治疗心衰的方法只能部分缓解心梗患者的症状,无法从根本上解决心梗后心肌细胞大量丢失的问题,所以业界对心脏再生医学寄予厚望。目前心脏再生领域仍存在许多未解决的问题,如尚未找到成年哺乳动物心脏干细胞,心脏细胞移植效率低且容易引起心律失常,心脏纤维细胞转分化为心肌细胞效率低等。同时,研究发现斑马鱼和乳鼠的心脏损伤后主要通过诱导心肌细胞增殖实现原位心脏再生,但是成年哺乳动物心肌细胞增殖率非常低,导致心脏损伤后不能再生。因此,提高成年哺乳动物内源性心肌细胞的增殖对心脏再生至关重要。然而目前已报道的基因、microRNAs(miRNAs)、化学小分子等诱导哺乳动物心肌细胞增殖的手段存在效率低、容易引起心律失常、需要依赖病毒作为递送工具等不足,不能满足临床转化需求。
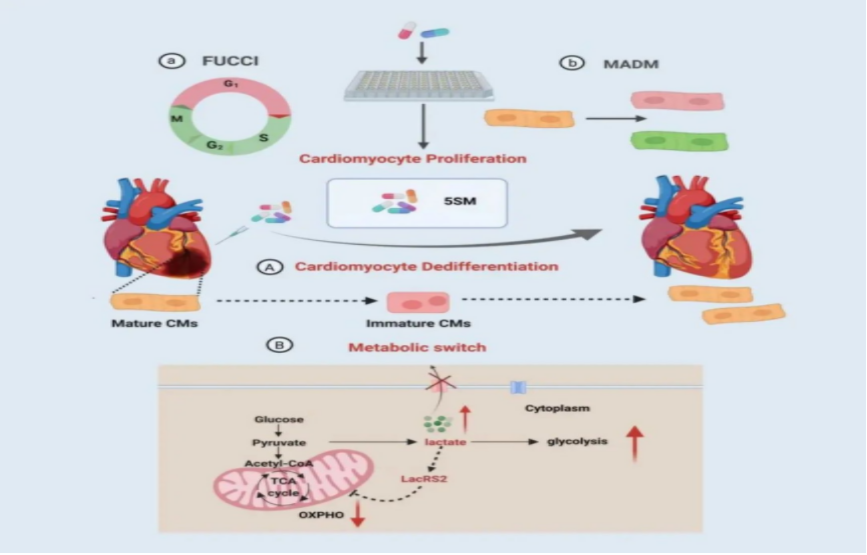
为了解决心脏再生重大难题,研究人员首先利用双荧光细胞周期报告系统FUCCI(标记有丝分裂S-G2-M期)和MADM(显示胞质分裂),以及一套高通量筛选系统,从化学小分子文库中筛选出13个能有效诱导心肌细胞进入细胞周期的小分子。值得一提的是,除MCT1抑制剂外,单个小分子基本不能诱导心肌细胞胞质分裂。因此研究者将单个小分子两两组合后验证其药效,并结合数学模型预测促增殖效果最佳的小分子组合,进一步通过体内、体外实验验证发现由盐酸去氧肾上腺素(α-adrenergic receptor激动剂)、巴瑞克替尼(JAK抑制剂)、去氢骆驼蓬碱(DRYK抑制剂)、VO-Ohpic trihydrate(PTEN抑制剂)和AZD3965(MCT1抑制剂)组成的小分子组合5SM,可成功诱导成年大、小鼠和人的心肌细胞重新进入细胞周期并且发生胞质分裂。随后研究人员建立大鼠心肌梗塞模型,发现5SM可显著改善成年大鼠心梗后的心脏功能,减少心脏纤维化面积。最后研究人员结合单细胞转录组测序(scRNA-seq)、ATAC-seq等组学和生物化学等技术,发现5SM诱导静止期的心肌细胞进入去分化状态,随后进入增殖状态;同时,5SM通过激活乳酸信号和mTOR通路,促进心肌细胞代谢由氧化磷酸化向糖酵解转换,最终诱导心肌细胞增殖和分裂(见下图)。该研究首次在国际上发现促进心脏原位再生的全小分子药物组合,揭示了心脏再生领域新的细胞和分子机制,为临床转化提供了新的候选小分子药物及新技术。
北京大学熊敬维教授、雷晓光教授以及复旦大学赵世民教授为共同通讯作者。北京大学未来技术学院博士研究生杜建勇(已经毕业)和郑丽霞为文章共同第一作者,中科院遗传发育所屠强研究员和杨航、同济大学魏珂教授和冯梦颖、复旦大学杨万洁、北京大学朱小君副研究员、高芃博士、郭富生、梁如琪、白林鹭、王子豪等对本文做出了重要贡献。该工作得到科技部“发育编程及其代谢调节”重点专项、国家自然科学基金委重点项目、阿斯利康(中国)、北京市卓越青年科学家计划、北京分子科学国家研究中心、北京大学分子医学南京转化研究院、北大-清华生命科学联合中心等多方面科研经费的资助。
原文链接:https://doi.org/10.1016/j.stem.2022.03.009
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#组合疗法#
114
#CEL#
80
#小分子#
106
#Cell#
110