J Stroke Cerebrovasc Dis:大血管硬化卒中患者的病理生理机制与预后
2015-08-20 phylis 译 MedSci原创
背景:缺血性脑卒中的病理学机制在长期预后的判断中起着重要的作用。我们主要调查由于大血管因素引起卒中的机制和长期预后之间的关系。方法:招募1993年-2010年间在雅典卒中登记的卒中患者,这些患者存在动脉粥样硬化。根据不同的发病机制,将病人分为3组:低血流量性梗塞,动脉栓子以及固有动脉粥样硬化组。随访时间长达10年或者直到死亡。研究的终点:10年死亡率,卒中再发率以及各种心血管事件的发生。结果:50
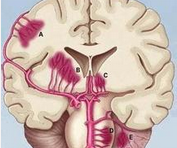
背景:缺血性脑卒中的病理学机制在长期预后的判断中起着重要的作用。我们主要调查由于大血管因素引起卒中的机制和长期预后之间的关系。
方法:招募1993年-2010年间在雅典卒中登记的卒中患者,这些患者存在动脉粥样硬化。根据不同的发病机制,将病人分为3组:低血流量性梗塞,动脉栓子以及固有动脉粥样硬化组。随访时间长达10年或者直到死亡。研究的终点:10年死亡率,卒中再发率以及各种心血管事件的发生。
结果:502名患者如下分组:156(31%)患者低血流量梗死,256 (51%) 患者动脑栓子梗塞,90 (18%)患者固有动脉粥样硬化。不同的梗死机制,10年的累积死亡率没有差异:低血流量组49.9% (95% CI, 38.5-61.3);动脉栓塞组47.6% (95% CI, 39.4-55.8);动脉粥样硬化组48.5% (95% CI, 34.0-63.0)。与动脉栓塞组患者,动脉粥样硬化组的患者的卒中再发率较高(HR = 2.1; 95% CI, 1.19-3.73)。与动脉栓塞组相比,动脉粥样硬化组和低血流量组患者的心血管事件发生率较高(HR 分别为1.94、1.64; 95% CI分别为 1.26-3.00,1.13-2.38)。
结论:低血流量组和动脉粥样硬化组卒中与未来心血管事件的发生和卒中的再发相关。然而,各组长期死亡率是相同的。
原文出处:
Psychogios K, Stathopoulos P, Takis K,et al. The Pathophysiological Mechanism Is an Independent Predictor of Long-Term Outcome in Stroke Patients with Large Vessel Atherosclerosis. J Stroke Cerebrovasc Dis. 2015 Aug 14.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
58
#Dis#
47
#血管硬化#
0
#卒中患者#
60
#病理生理#
71
#大血管#
60
我喜欢我喜欢
144