诺华公布新获批抗癌药Zykadia积极数据
2014-06-05 佚名 生物谷
诺华(Novartis)6月2日公布了抗癌药Zykadia(ceritinib,LDK378)的积极数据。数据表明,Zykadia缩小了间变性淋巴瘤激酶阳性(ALK+)非小细胞肺癌(NSCLC)患者的肿瘤体积,包括那些既往接受过ALK抑制剂治疗的患者群体以及ALK抑制剂初治患者群体。此外,Zykadia也缩小了ALK+NSCLC脑转移肿瘤的体积。相关数据已提交至美国临床肿瘤学会(ASCO)第5

诺华(Novartis)6月2日公布了抗癌药Zykadia(ceritinib,LDK378)的积极数据。数据表明,Zykadia缩小了间变性淋巴瘤激酶阳性(ALK+)非小细胞肺癌(NSCLC)患者的肿瘤体积,包括那些既往接受过ALK抑制剂治疗的患者群体以及ALK抑制剂初治患者群体。此外,Zykadia也缩小了ALK+NSCLC脑转移肿瘤的体积。相关数据已提交至美国临床肿瘤学会(ASCO)第50届年会。
在所有246例NSCLC患者中,Zykadia取得了58.5%的整体反应率(ORR),平均无进展生存期为8.2个月。其中有124例患者在参与研究时肿瘤已脑转移,该患者群体的ORR为54.0%,PFS为6.9个月。
基于该项研究的数据,FDA于今年4月批准Zykadia(ceritinib),用于经Xalkori(crizotinib)治疗后病情恶化或对Xalkori不耐受的间变性淋巴瘤激酶阳性(ALK+)转移性非小细胞肺癌(NSCLC)患者的治疗。此前,FDA已授予Zykadia突破性疗法认定。
对于启动Xalkori初步治疗后病情复发的ALK+NSCLC患者群体,Zykadia将是一个重要的治疗选择,将解决这一群体中未获满足的医疗需求。
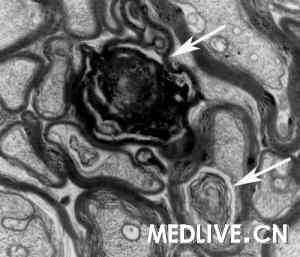
肺癌是导致癌症死亡的主要原因之一。非小细胞肺癌(NSCLC)占到了肺癌病例的85%-90%,其中2%-7%病例由ALK基因的重排(rearrangement)所驱动,导致癌细胞的加速生长。尽管ALK+NSCLC群体的临床治疗已取得显著进展,但病情恶化往往是不可避免的,因此需要更多的治疗选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#积极数据#
60
#DIA#
42
#诺华#
63
#抗癌药#
64