实验性关节炎药物可预防干细胞移植并发症
2018-04-27 MedSci MedSci原创
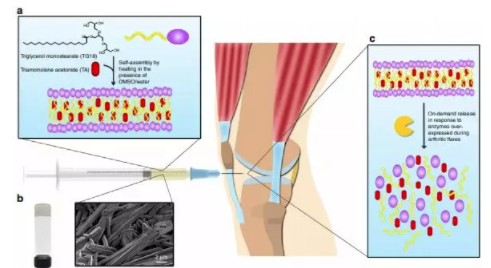
近日,华盛顿大学圣路易斯医学院的一项最新研究显示,一种用于类风湿性关节炎的临床试验中的药物可以预防干细胞移植的危及生命的并发症。以小鼠为模型,研究人员发现这种药物能够阻止移植物抗宿主病,这是一种使移植的干细胞攻击受移植患者自身器官或组织的致命性疾病。
近日,华盛顿大学圣路易斯医学院的一项最新研究显示,一种用于类风湿性关节炎的临床试验中的药物可以预防干细胞移植的危及生命的并发症。以小鼠为模型,研究人员发现这种药物能够阻止移植物抗宿主病,这是一种使移植的干细胞攻击受移植患者自身器官或组织的致命性疾病。
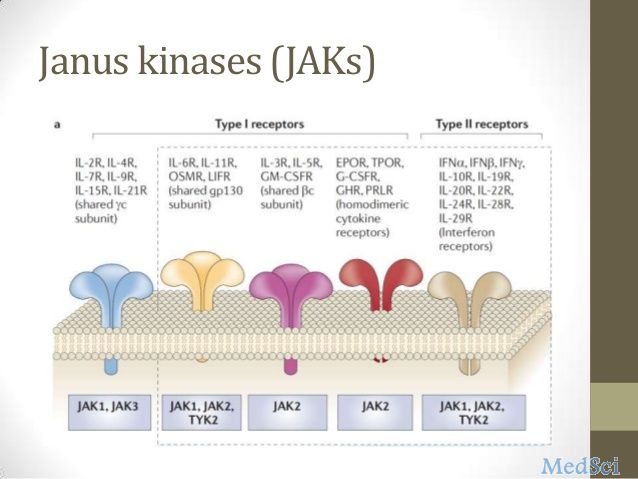
大约一半的接受供体干细胞移植的患者会发生移植物抗宿主病,移植物可能在移植后持续数月或数年产生疾病反应。在某些情况下,患者的死亡往往是因为移植物抗宿主病。在过去的工作中,该研究小组确定了JAK1 / 2激酶的分子作用及其在免疫细胞活化和移植物抗宿主病中的信号传导途径。在这项新研究中,这些研究人员评估了ruxolitinib和baricitinib,发现这两种药物在降低和预防小鼠移植物抗宿主病方面具有显著优势。
本研究的高级作者John F. DiPersio博士说:“移植供体干细胞,特别擅长治疗白血病,但不幸的是,这些细胞可能会失去控制,并攻击患者的健康组织,从而导致移植物抗宿主疾病。我们正在寻找一种治疗策略,在不关闭T细胞对癌症的攻击的情况下阻止疾病的发生”。令人惊讶的是,baricitinib不仅防止了移植物抗宿主病,它实际上也增强了供体T细胞对抗肿瘤细胞的能力。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/75302/drug-prevents-stem-cell-transplant/
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#实验性#
107
#关节炎药物#
92
#并发#
68
#细胞移植#
61
#关节炎#
63