Cancer cell:华人科学家发现遏制恶性肿瘤生长新策略
2015-11-19 佚名 生物谷
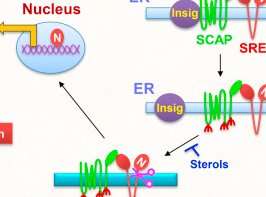
本文研究亮点: SCAP是一个葡萄糖应答蛋白,能量供应与SREBP激活通过SCAP联系在一起 SCAP蛋白发生N-糖基化能够促进SCAP/SREBP从内质网向高尔基体运输 EGFR通过促进葡萄糖转运以及SCAP蛋白N-糖基化激活SCAP/SREBP 靶向SCAP蛋白N-糖基化是一种非常具有前景的恶性肿瘤治疗方法

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#cancer cell#
72
#CEL#
67
#Cell#
61
#科学家发现#
68
#新策略#
67
#华人#
79