Blood:维甲酸反应性CD8效应T细胞在胃肠GvHD富含IL-23的组织中选择性扩增
2020-09-22 MedSci原创 MedSci原创
维甲酸主要增加同种异体反应性的RARahi CD8效应T细胞,包括体内鉴定的表型细胞。IL-23可通过选择性增加CD8效应T细胞上b7整合素的表达和降低具有调节细胞表型的CD4 T细胞来加强这一效应。
胃肠道(GI)移植物抗宿主病(GvHD)是异基因造血干细胞移植(AHST)的主要障碍。代谢产物维甲酸(RA)通过表达RA受体α(RARα)的同种反应性T细胞增强小鼠的GI-GvHD,但RA反应性细胞在人GI-GvHD中的作用尚不清楚。
在本研究中,Ball等使用传统的和新型序贯免疫染色和流式细胞术来仔细观察AHST患者组织和血液中的RA反应性T细胞,并表征RA对人类T细胞同种异体反应的影响。
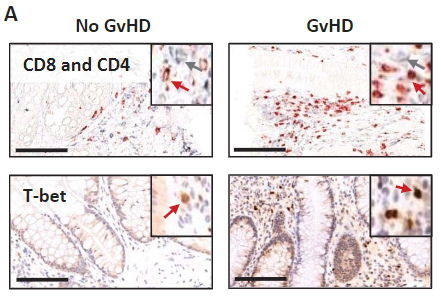
(在GI-GvHD组织中,RARαhi单核细胞数量增多)
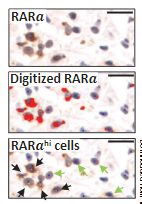
在RA暴露后,人单个核细胞RARα的表达水平增加。在GI-GvHD组织中,RARαhi单核细胞数量增多,这些细胞内的RA结合蛋白增多,定位于组织损伤的地方,与GvHD的严重程度和病死率相关。
(在GvHD组织中,T-bet的表达增多)
通过靶向候选蛋白方法,研究人员预测了在微环境IL-23增加的情况下RA反应性T细胞的表型。序贯免疫染色证实了存在一群具有预测表型的RARahi CD8T细胞,共表达效应T细胞转录因子T-bet和IL-23特异性受体。这些细胞在GI-GvHD组织中增加,但在皮肤-GvHD组织中没有增加,并且在GI-GvHD患者的血液中有选择性地扩增。
最后,功能研究显示,RA主要增加同种异体反应性的RARahi CD8效应T细胞,包括体内鉴定的表型细胞。富含IL-23的条件可通过选择性增加CD8效应T细胞上b7整合素的表达和降低具有调节细胞表型的CD4 T细胞来加强这一效应。
总之,Ball等鉴定出了一组具有独特表型的RA反应性效应T细胞,它们在人GI-GvHD中选择性扩增,可作为潜在的新的治疗靶点。
原始出处:
Ball Jennifer A,Clear Andrew James,Aries James et al. Retinoic acid-responsive CD8 effector T-cells are selectively increased in IL-23-rich tissue in gastrointestinal GvHD. Blood, Sep 09 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#反应性#
75
#选择性#
68
学习了很不错,每天都要来学习一下
131
#IL-23#
116
#CD8#
71
#IL-2#
99
学到了
160