HIV免疫疗法获重大突破,一览研究进展
2017-04-19 小博 医麦克
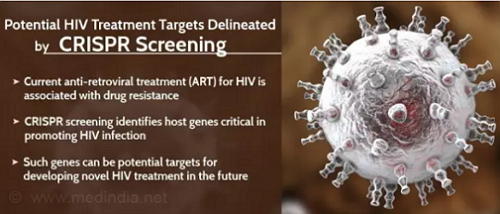
近日,关于HIV免疫疗法迎来了两项新突破。来自美国TSRI和中国上海科技大学的研究人员成功构建出抵抗HIV的免疫细胞,有望治愈HIV感染;美国天普大学华人科学家胡文辉等人利用基因编辑技术,从多靶点高效剔除了一种人源化小鼠多个器官组织中的人类HIV病毒。近日,关于HIV免疫疗法迎来了两项新突破:来自美国TSRI和中国上海科技大学的研究人员成功构建出抵抗HIV的免疫细胞,有望治愈HIV感染;美国天


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习
0
学习
93
学习
107
学习
105
学习
113
学习
52
学习
47
学习
60
学习
48
#研究进展#
52