Eur Heart J:接受PCI的高出血风险患者替格瑞洛单药治疗效果分析
2021-10-20 MedSci原创 MedSci原创
在完成3个月DAPT且未出现重大不良事件的接受PCI的HBR患者中,与替格瑞洛联合阿司匹林治疗相比,停用阿司匹林后进行替格瑞洛单药治疗可显著减少出血,而不会增加缺血事件。
在接受经皮冠状动脉介入治疗(PCI)的患者中,高出血风险(HBR)患者是一个常见的亚组。在短期双重抗血小板治疗(DAPT)后尽早停用阿司匹林已成为一种避免出血的策略。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究的目的是评估3个月DAPT后替格瑞洛单药治疗对当代HBR人群的影响。

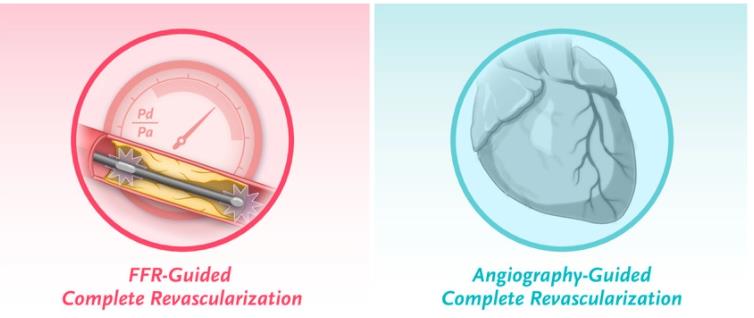
这项对TWILIGHT试验的预设分析评估了在接受PCI和药物洗脱支架的HBR患者早期停用阿司匹林后使用替格瑞洛单药治疗的治疗效果。替格瑞洛加阿司匹林治疗3个月后,无事件患者被随机分配至12个月的阿司匹林或安慰剂加替格瑞洛治疗。

该研究共有1064名(17.2%)患者符合学术研究联盟对HBR的定义。在HBR患者(6.3% vs. 11.4%;风险比(HR)为0.53,95%置信区间(CI)为0.35-0.82)和非HBR患者(3.5% vs. 5.9%;HR为0.59,95%CI为0.46–0.77)中,与替格瑞洛联合阿司匹林治疗相比,替格瑞洛单药治疗降低了出血学术研究联盟(BARC)2、3或5级出血的主要终点发生率(相互作用P=0.67),且在两者之间疗效相似,但前者的绝对风险降低趋势更大[-5.1% vs. -2.3%;绝对风险差异(ARDs)为-2.8%,95%CI为-6.4%至0.8%,P=0.130]。对于更严重的BARC3或5级出血,研究人员观察到了类似的模式,在HBR患者中绝对风险降低更大(-3.5% vs. -0.5%;ARDs差异为-3.0%,95%CI为-5.2%至-0.8%,P=0.008)。无论HBR状态如何,治疗组之间的死亡、心肌梗塞或卒中等关键次要终点没有显著差异。
在完成3个月DAPT且未出现重大不良事件的接受PCI的HBR患者中,与替格瑞洛联合阿司匹林治疗相比,停用阿司匹林后进行替格瑞洛单药治疗可显著减少出血,而不会增加缺血事件。HBR患者大出血的绝对风险降低幅度大于非HBR患者。
原始出处:
Javier Escaned.et al.Ticagrelor monotherapy in patients at high bleeding risk undergoing percutaneous coronary intervention: TWILIGHT-HBR.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab702
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#单药治疗#
87
#治疗效果#
75
#效果分析#
125
#ART#
75
#高出血风险#
65
#HEART#
70