Ann Surg:AS-DD术式治疗长段Barrett食管的远期(18年)预后!
2021-01-25 MedSci原创 MedSci原创
Barrett食管(BE)是慢性胃食管反流病(GERD)的一种危险并发症
Barrett食管(BE)是慢性胃食管反流病(GERD)的一种危险并发症,其特征是正常鳞状上皮细胞被柱状黏膜(CLM)以及有杯状细胞的肠上皮化生(IM)取代,是目前唯一已知的食管腺癌(EAC)的癌前病变。
大多数非肥胖的BE患者都采用Nissen胃底折叠术治疗,然而,Nissen胃底折叠术已被证明不能阻止Barrett食管的混合反流。该前瞻性研究旨在评估酸抑制-十二指肠分流(AS-DD)手术(包括选择性迷走神经切断术、胃底折叠术、胃大部切除+Roux-en-Y重建术)治疗长段BE(LSBE)和超长段BE(ELSBE)的远期疗效,以确定AS-DD手术对肠化生和进展为EAC的组织学影响。
研究流程
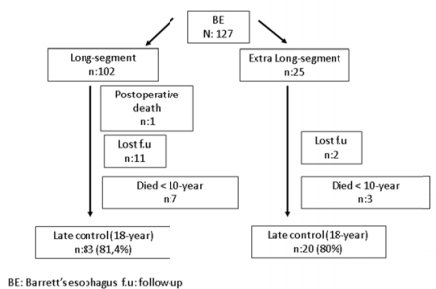
共招募了127名受试者,其中LSBE和ELSBE分别有102例和25例。81%的病例平均随访了18年。
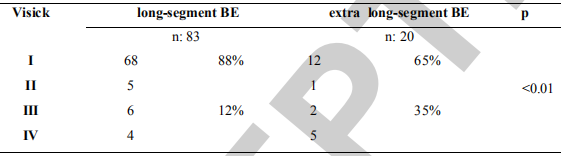
术后Visick评分
LSBE组88%的病例为Visick评分I-II级,ELSBE组的是65%的病例(P<0.01)。糜烂性食管炎和食道消化性溃疡明显愈合,71%的狭窄消失。LSBE组中有38%的IM病例转归。两组各有2例进展为EAC,平均历时15年。病理性胃酸反流治愈率为91%,十二指肠反流治愈率为100%。80%的低度异型增生消退为IM。
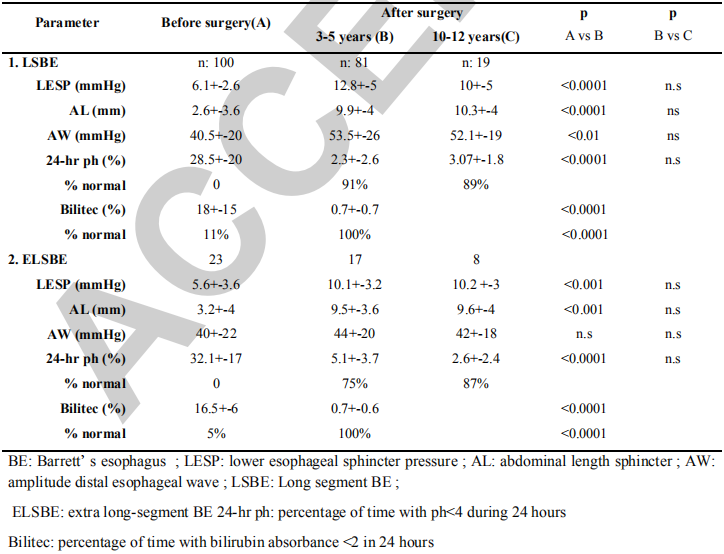
手术前后的功能性评估
综上,AS-DD可永久消除病理性食管反流。与内科治疗相比,采用AS-DD治疗的进展成HGD/EAC的风险较低,LSBE的风险降低了8倍,ELSBE的降低了2.2倍。AS-DD似乎可影响IM的行为,是一个可以减少和延缓EAC进展的有效治疗方式。
原始出处:
Csendes Attila,Orellana Omar,Figueroa Manuel et al. Long-term (18 Years) Results of Patients With Long-segment Barrett's Esophagus Submitted to Acid Suppression-duodenal Diversion Operation: Better Than Nissen Fundoplication? Ann Surg, 2021, 10.1097/SLA.0000000000004760.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#RET#
92
这就很nice
112
#Barrett食管#
96
#食管#
63
#Barrett#
80