Cell Metab:科学家发现攻克1型和2型糖尿病的关键机制
2017-03-14 生物谷 生物谷
如果身体出现胰岛素抵抗,胰腺会产生更多β细胞来进行胰岛素合成。研究人员一直想要弄清楚对于糖尿病前期或糖尿病患者来说这些细胞为何经常无法正常增殖,加斯林糖尿病中心的科学家们通过对人和小鼠进行研究发现了一个阻止细胞成功分裂的关键生物学机制。之前关于β细胞增殖的研究通常都聚焦在影响细胞周期的机制上。“成年哺乳动物的β细胞处于一种静息状态,因此如果

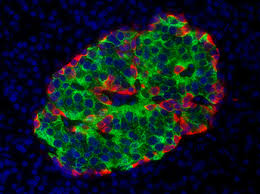
如果身体出现胰岛素抵抗,胰腺会产生更多β细胞来进行胰岛素合成。研究人员一直想要弄清楚对于糖尿病前期或糖尿病患者来说这些细胞为何经常无法正常增殖,加斯林糖尿病中心的科学家们通过对人和小鼠进行研究发现了一个阻止细胞成功分裂的关键生物学机制。
之前关于β细胞增殖的研究通常都聚焦在影响细胞周期的机制上。“成年哺乳动物的β细胞处于一种静息状态,因此如果你想把它们推进细胞周期,你就需要将它们唤醒。”哈佛大学医学院教授Kulkarni这样解释道。在过去的几年里科学家们已经发现了许多帮助启动细胞周期的生物学机制。
为了找到β细胞无法正常分裂的原因,Kulkarn教授实验室曾经对缺失了胰岛素受体的β细胞进行分析,这些细胞并不能像正常β细胞一样分裂。在他们发现的结果当中,科学家们发现这些细胞相比于正常细胞来说有两种蛋白的表达量比较低,这两种蛋白能够在细胞分裂之前帮助将细胞内的染色体分开。
在这项最新研究中,研究人员在小鼠模型以及人和小鼠的细胞中对这两个蛋白——CENP-A和PLK1进行了研究。“我们发现缺失了CENP-A的小鼠无法通过产生更多的胰岛素分泌细胞来对胰岛素抵抗进行补偿。”Kulkarni这样说道。
除此之外他们还对人类β细胞进行了检测,发现糖尿病患者提供的细胞中CENP-A和PLK-1这两个蛋白的表达水平比健康人更低。
为了更好地理解胰岛素信号如何影响β细胞生长,研究人员又研究了FOXM1参与的一个信号途径。该蛋白作为一个转录因子调节基因表达,能够帮助驱动细胞增殖,促进CENP-A和PLK-1的表达。
“我们发现胰岛素信号可以启动这个转录因子与CENP-A和PLK-1基因的结合,而在缺失了胰岛素受体的β细胞中缺少这种结合,导致细胞死亡而不是分裂。” Kulkarni这样说道。
“我们还发现这种调控只存在于β细胞,在其他代谢相关细胞类型,比如肝脏细胞和脂肪细胞中并未发现。”
在了解到β细胞如何分裂以及分裂如何受到阻碍之后,下一步就是研究能否靶向FOXM1或该途径的其他蛋白通过推动细胞周期产生更多β细胞。该研究可能不仅掌握了2型糖尿病的治疗希望,也对1型糖尿病的治疗有重要提示。
原始出处:
Jun Shirakawa,Insulin Signaling Regulates the FoxM1/PLK1/CENP-A Pathway to Promote Adaptive Pancreatic β Cell Proliferation.Cell Metabolism.2017.02.004
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
76
#MET#
64
#Cell#
66
#科学家发现#
64
#Meta#
65
胰岛素抵抗下,身体认为过多胰岛素没用,从而减少β细胞增值,这不也是一种代偿反应吗?---另,产生更多的β细胞,产生更多胰岛素,是否会加剧抵抗反应呢?
130