Eur J Radiol:使用脑血流量权重的动脉自旋标记MRI发现卒中后小脑失联络
2016-04-16 MedSci MedSci原创
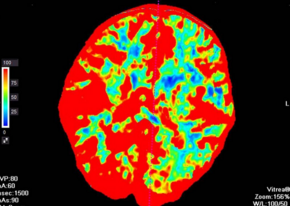
研究背景及研究目的:小脑失联络是血流动力学PET和SPECT最常发现的影像,然而非创伤的MRI有更高的空间分辨率,允许血流动力学改变和直接的结构学发现相比较,而没有电离辐射暴露的担心,这项研究的目的在于评价通过脑血流量权重的动脉自旋标记MR及脑血管反应性权重的血氧水平依赖的MRI确定的小脑失联络和华勒变性,临床运动缺损及皮质脊髓束累及之间的关系。 &nbs
研究背景及研究目的:小脑失联络是血流动力学PET和SPECT最常发现的影像,然而非创伤的MRI有更高的空间分辨率,允许血流动力学改变和直接的结构学发现相比较,而没有电离辐射暴露的担心,这项研究的目的在于评价通过脑血流量权重的动脉自旋标记MR及脑血管反应性权重的血氧水平依赖的MRI确定的小脑失联络和华勒变性,临床运动缺损及皮质脊髓束累及之间的关系。
研究方法:74例入组一项不间断的观察性的卒中试验进行脑血流量权重的动脉自旋标记MR和高碳酸学的脑血管反应活性权重的血氧水平依赖的MRI。在18例单边幕上梗死的病人和16例无梗死的对照比较其小脑基底部脑血流量、脑血管反应性,脑腔梗区域的脑半球不对称性。
研究结果:在9例小脑失联络的病例中,脑血管反应性(p=0.04)和脑腔梗区域(p<0.01)与对照组相比具有显著的双侧不对称性。和梗死却没有小脑失联络的9例患者相比小脑失联络的患者在梗死在皮质脊髓束定位(p=1.0)和运动缺损(p=0.08)中没有差别。
研究结论:小脑失联络和小脑脑血管反应性不对称性及华勒变性相关。这些发现表明非创伤的MRI可能是研究幕上脑梗后小脑失联络的临床结局及结构因素的除PET和SPECT的另一选择。
原始出处:
Strother MK1, Buckingham C1, Faraco CC1, Arteaga DF1, Lu P2, Xu Y2, Donahue MJ3.et al,Crossed cerebellar diaschisis after stroke identified noninvasively with cerebral blood flow-weighted arterial spinlabeling MRI.Eur J Radiol. 2016 Jan;85
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#脑血流#
60
#卒中后#
51
#动脉自旋标记#
64
#动脉自旋标记MRI#
57
#血流量#
58