JCO:抗VEGFR-TKI耐药也不怕,卡博替尼治疗末线分化型甲状腺癌仍有很好的疗效
2017-08-24 王东亮 肿瘤资讯
甲状腺癌是很常见的内分泌肿瘤,且发病率在逐年上升,大多数患者发病年龄较轻,约2/3患者年纪小于55岁,女性患者居多。尽管甲状腺癌预后较好,约90%患者都可获得长期生存,但进展期肿瘤或碘耐药的部分患者治疗效果仍不甚理想。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JCO#
73
学习一下很不错
114
#分化型甲状腺癌#
76
#VEGF#
52
#EGFR-TKI#
60
#TKI#
72
#VEGFR#
70
#GFR#
67
#抗VEGF#
70
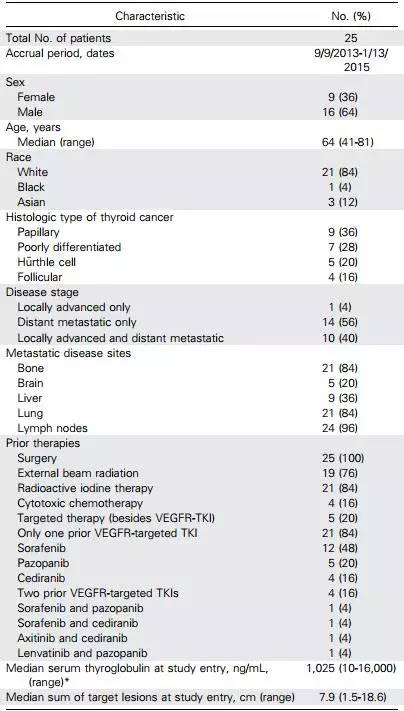
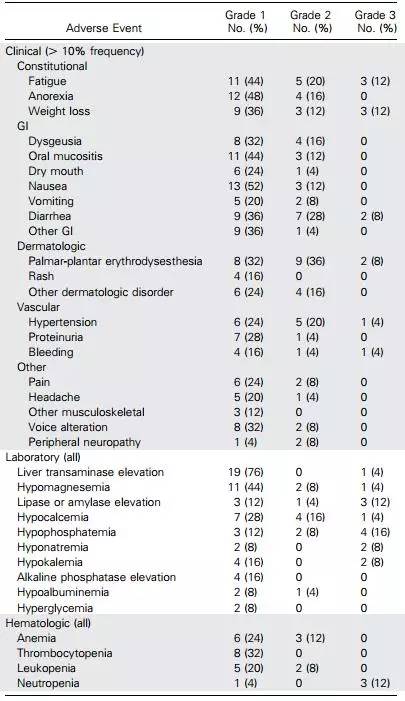
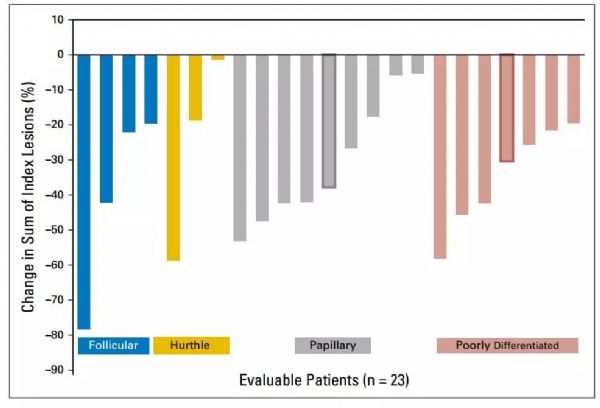
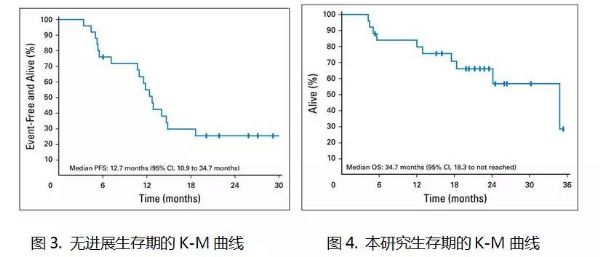
先前1-2线抗VEGFR失败的末线分化型甲状腺癌临床研究.本研究结果证实卡博替尼治疗末线患者依然有效.客观缓解率可高达40%.中位无进展生存期12.7个月.无进展生存期34.7个月.
124