Heart:先心病患儿的很大摄氧量明显低于正常儿童
2018-06-03 MedSci MedSci原创
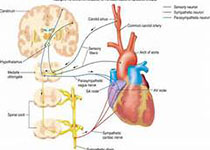
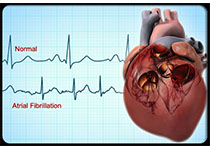
本研究的目的旨在评估先天性心脏病患儿的心肺功能与正常健康同龄儿童之间的差异,并寻找与最大摄氧量(VO2max)相关的临床特征。本次多中心横断面研究纳入了798名儿童(496名先心病患儿和302名正常儿童),并对其进行了完整的心肺功能测试(CPET)。分析结果显示,先心病组和对照组的平均VO2max预测值分别为93%±20%和107%±17%,先心病患儿的VO2max要明显更低(37.8±0.3vs
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#先心病#
66
#ART#
73
#HEART#
63
学习了.谢谢作者分享!学习了.谢谢作者分享!
132
陈v该好好还好还好哈
118