AJG: 新末端回肠的术后内镜复发是克罗恩病的长期预后预测因素
2020-07-03 MedSci原创 MedSci原创
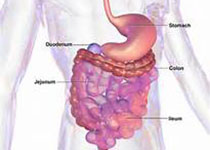
克罗恩病患者术后第一年内进行早期回肠结肠镜检查是评估回肠结肠切除术克罗恩病(CD)复发率的金标准。本项研究的目的是评估术后早期结肠镜检查中吻合口和回肠病变的存在与严重程度与疾病长期预后之间的关系。
背景及目的:
克罗恩病患者术后第一年内进行早期回肠结肠镜检查是评估回肠结肠切除术克罗恩病(CD)复发率的金标准。本项研究的目的是评估术后早期结肠镜检查中吻合口和回肠病变的存在与严重程度与疾病长期预后之间的关系。
方法:
本项研究是一项前瞻性多中心研究,纳入了包括接受回肠或回结肠CD手术的患者,所有患者术后6个月进行结肠镜检查。研究人员分别建立了描述吻合和回肠病变的内窥镜评分。临床复发是由CD相关症状定义的,并通过影像学,内窥镜检查或治疗强化证实。
结果:
在225名患者中,有193名接受了长期随访(中位随访时间:3.82年)。中位无复发生存期为47.6个月。与无回肠病变的患者(I(0))相比,术后早期内镜下有回肠病变的患者无论其严重程度为(I(1)或I(2,3,4)),其临床无复发生存期均明显缩短( I(0)vs I(2,3,4):P = 0.0003; I(0)vs I(1):P = 0.0008和I(1)vs I(2,3,4):P = 0.43) 。仅具有回肠病变的患者(A(0)I(1,2,3,4))的临床长期结局要比仅具有回肠病变的患者(A(1,2,3)I(0))(P = 0.009)要好。
讨论:
本项研究证实对克罗恩病术后患者分别描述吻合口和回肠病变的评分可能更适合定义术后内镜复发。治疗具有回肠病变的患者(包括轻度回肠病变(I(1)))以改善长期预后。
原始出处:
Hammoudi, Nassim. Et al. Postoperative Endoscopic Recurrence on the Neoterminal Ileum But Not on the Anastomosis Is Mainly Driving Long-Term Outcomes in Crohn's Disease. The American Journal of Gastroenterology. 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AJG#
78
#长期预后#
0
腻害腻害
115
#内镜#
80
#预测因素#
68
#回肠#
74
学习了。
138