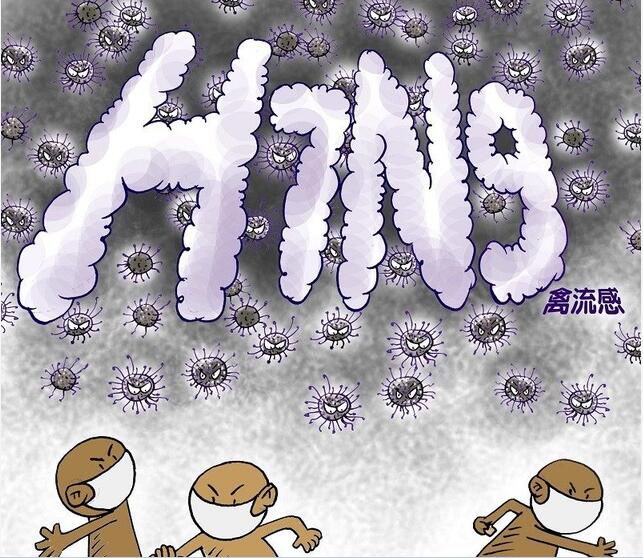
国际组织:警惕 H7N9 禽流感致病性增高
2017-03-20 佚名 新华社
鉴于近期人类感染H7N9禽流感病例数量明显增多,世界动物卫生组织与联合国粮农组织17日发表联合公报,提醒各国警惕H7N9亚型病毒因基因变异而对禽类致病性增高,呼吁加强对禽流感疫情动物源头的防控和诊断,以防止病毒进一步蔓延,减少对人类健康的威胁。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#致病性#
97
学习了,分享了学
94
#H7N9#
51
#增高#
79
#增高#
61