JACC Cardiovasc Imag:无症状性心肌梗死的发病特点及预后
2018-12-18 国际循环编辑部 国际循环
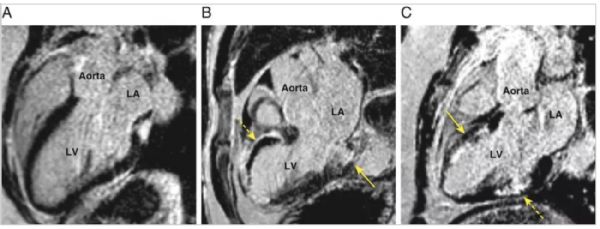
近日,JACC: Cardiovascular Imaging发表一项研究,调查首次急性心肌梗死(AMI)发病患者的无症状性心肌梗死(SMI)患病率及其与长期随访时死亡率和主要不良心血管事件(MACE)的关系。既往研究表明,高达54%的MI发生时无明显症状,但SMI对首次AMI患者发病率和长期预后的意义尚不清楚。 研究纳入2003年~2013年首次AMI发病的392例患者,其在AMI后1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
56
#ASC#
74
好
88
#ACC#
65
#无症状#
74
很好的学习机会
86
8.2%的发生率,由于没有引起重视这部分人群,更是高危亚组。
84
无症状心肌梗死
90
谢谢了,学习
92
学习了,谢谢分享。
67