伊布利特(Ibutilide)在持续性心房颤动消融中的应用
2011-05-07 MedSci原创 MedSci原创
杨 龙 贵州省人民医院 伊布利特的电生理机制和适用范围 伊布利特(Ibutilide,Ibu)是一种Ⅲ类AAD,可延长动作电位时程和有效不应期,其主要电生理机制为:①抑制复极相k+外向电流;②促进平台期缓慢内向Na+电流;③促进平台期内向Ca2+电流。由于Ibu对心房肌的作用较心室肌显著,因此,临床上主要应用于快速房性心律失常的治疗,尤其是转复新发AF和房扑,
杨 龙 贵州省人民医院 伊布利特的电生理机制和适用范围
伊布利特(Ibutilide,Ibu)是一种Ⅲ类AAD,可延长动作电位时程和有效不应期,其主要电生理机制为:①抑制复极相k+外向电流;②促进平台期缓慢内向Na+电流;③促进平台期内向Ca2+电流。由于Ibu对心房肌的作用较心室肌显著,因此,临床上主要应用于快速房性心律失常的治疗,尤其是转复新发AF和房扑,具有安全、快速、高效的特点。近年来Ibu使用范围有所增加,渐有应用于持续AF复律以及AF消融术中的报道。
Ibu对临床阵发性AF的转复率达61.5%~77%,而对持续性AF转复率仅41.1%~48%。在与胺碘酮和普罗帕酮的对比研究中,Ibu对90天内发生的AF的转复率与二者相近,或优于后者。AF射频消融术中使用Ibu复律的相关报道极少。Nademanee等在AF消融后使用Ibu转复遗留的 LAFL和AT,慢性AF患者的转复率为75%(18/24)。Oral等在环肺静脉隔离消融术后行体外同步电复律转为SR而又在60 s内复发AF的患者中,静注Ibu 1 mg转复成功率为60%(9/15)。
伊布利特在持续性AF消融中的研究
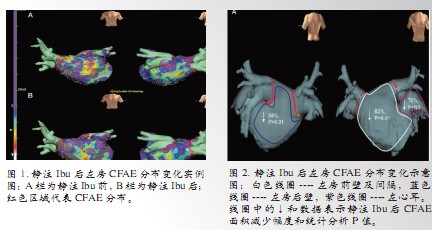
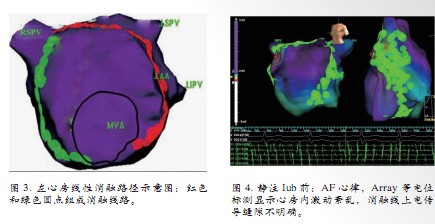
Singh等首先报道(亦是笔者所见迄今唯一的报道)在持续AF消融术中使用Ibu辅助消融,达到延长AA间期、优化碎裂电位(CFAE)的目的,从而利于导向CFAE消融。该研究纳入11例患者,年龄55±6岁,左房前后径48±15 mm,AF持续时间0.5~18年(中位数3年)。完成环肺静脉隔离后,行CFAE标测,激动周长(AA间期)<120 ms区域定义为CFAE区。静脉注射Ibu后再行CFAE标测,平均心房激动周期由用药前146 ms延长至用药后165 ms (P=0.01);左房CFAE分布部位无明显变化,但分布区域面积明显缩小(图1,2)。针对优化后的CFAE消融,共9(81.8%)例AF转复为 SR,1例AT和1例AF行体外同步电复律转为SR。随访62??733天(中位数455天),8(72%)例无AF/AT发作,未服用AAD。3例接受二次消融,其中1例二次消融后无AF/AT发作。复发的3例患者中仅1例需服用Dofetilide以减少AF/AT复发从而缓解症状,其余2例因复发不频繁、持续时间短、症状轻而未服用AAD。
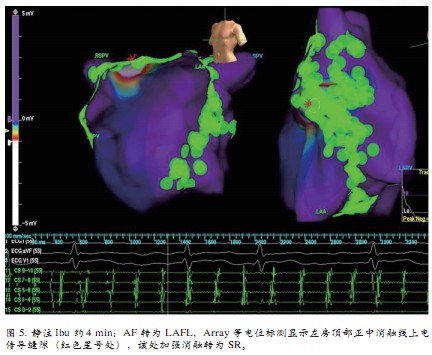
阜外心血管病医院姚焰等自2年前开始,在持续性AF线性消融术中使用Ibu辅助转复经充分消融仍残留的AF和LAFL。迄今纳入持续AF患者65例,年龄 54.1±8.4岁,左房前后径40.7±5.3 mm,AF持续时间10天??11年(中位数1年)。纳入标准为:行左房线性消融(消融线路见图3),消融线完整相连,线上记录不到心房电位或电位较消融前减小至少90%,并针对线上缝隙消融累计不少于10 min 后AF或LAFL仍不终止者。给予富马酸伊布利特注射液1 mg以0.2 mg/min静脉注射,重复给药需间隔10 min,总量≤2 mg。待AA间期明显延长或AF转为LAFL或AT之后重新标测,针对消融线上缝隙加强消融。总结Ibu具有三方面作用:①药效复律:部分患者给药后未经加强消融即转复为SR;②辅助消融线上残留电传导缝隙(gap)的定位,导向加强消融:给药后AA间期延长且相对整齐,或者AF转为 LAFL,Ensite Array等电位标测显示消融线上缝隙愈加清楚,使得加强消融部位更加明确(见图4,5);③提高电复律的成功率:给药并加强消融仍未恢复SR者,体外同步电复律一次成功率为84.6%(11/13)。同时,Ibu具有以下特点:①高效:给药后结合加强消融,72.3%(47/65)的患者成功转为 SR;②快捷:转复时间10.8±9.6 (2.0~41) min;③安全:平均用药量为1.06 (0.4~2.0)mg,给药后观察12 h,未见严重药物副作用(如多形性室性心动过速、严重心动过缓、严重低血压)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








That's a sharp way of thinikng about it.
166
#持续性#
72
#消融#
67
#心房#
77