Cell揭秘:癌细胞如何对抗“免疫疗法”?靠突变! 大牛夫妇新作
2016-09-25 佚名 生物探索
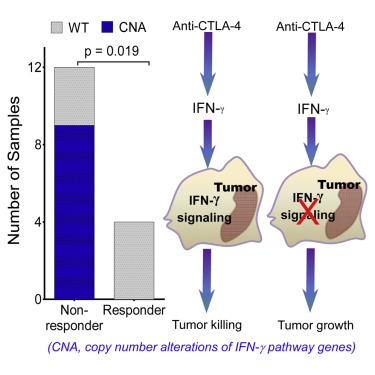
Cell揭秘:导语:德克萨斯大学安德森癌症中心免疫学系主任James P.Allison教授是癌症免疫疗法的先驱之一,也被称CTLA-4抗体“Yervoy之父”。这款在2011年获FDA批准的免疫疗法抗体挽救了无数癌症患者的生命。9月21日,Allison教授荣获了有着诺奖风向标之称的汤森路透“引文桂冠奖”。相隔1天,这位大牛又在Cell杂志上发表了一项重要成果,揭秘了癌细胞对抗免疫疗法的关键



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
39
感谢博士的讲解!分享一下!
86
感谢博士的讲解!
83
#Cell#
40
总结的很好!
105
分享一下!
99
分享一下!
96
总结的很好!!
33
有大量的临床试验在开发它作为单药或联合其它药物治疗多种类型的癌症!!!
40
分享一下!!
38