AJG:Fibrosis-4指数可以独立预测非酒精性脂肪肝的主要心血管不良事件的发生率
2022-02-23 MedSci原创 MedSci原创
非酒精性脂肪性肝病(NAFLD)是指除外酒精和其他明确的损肝因素所致的肝细胞内脂肪过度沉积为主要特征的临床病理综合征,与胰岛素抵抗和遗传易感性密切相关的获得性代谢应激性肝损伤。
非酒精性脂肪肝(NAFLD)是全球最常见的慢性肝病,预计到2030年,受影响的人数将超过1亿人。非酒精性肝病包括一系列的肝脏病变,包括简单的脂肪堆积(5%以上的肝细胞中的单纯脂肪堆积(脂肪病)、脂肪堆积和炎症(脂肪性肝炎,NASH)、纤维化,以及在没有过度饮酒的情况下最终导致肝硬化。非酒精性脂肪肝是一种多系统的疾病,与心血管疾病(CVD)密切相关。非酒精性脂肪肝患者不仅遭受非致命性心血管(CV)事件的风险更高,而且更有可能经历心血管疾病相关的死亡风险。非酒精性脂肪肝的危险因素包括糖尿病和肥胖,这也是公认的心血管疾病的危险因素。而且越来越多的证据表明,非酒精性脂肪肝是一个独立的心血管疾病风险因素。对非酒精性脂肪肝患者进行筛查和风险分层,应该是护理标准的一部分。然而,与普通人群相比,目前几乎没有有效的工具来对非酒精性脂肪肝患者的心血管风险进行分层。纤维化-4指数(FIB-4)是一个易于计算、广泛使用的临床评分。它主要由包括年龄、天冬氨酸氨基转移酶、丙氨酸氨基转移酶(ALT)和血小板的不同权重积分构成。最近的数据表明,FIB-4有可能成为非酒精性脂肪肝患者的肝脏相关结果、CV风险和死亡率的预后评分。然而,FIB-4和主要不良心血管事件(MACE)之间的关系还没有在大规模的研究中得到调查。因此,本项研究旨在确定纤维化 4 指数 (FIB-4) 是否可以识别出心血管事件风险最高的 NAFLD 患者。

为了完成本项研究,研究人员总共纳入了81,108 名患者的数据,这些患者主要分为3类 (i) 诊断为 NAFLD,(ii) 非酒精性脂肪性肝炎 (NASH),或 (iii) 有 NASH 风险 (RISK)。主要观察结果是主要不良心血管事件 (MACE)的发生,其定义为心肌梗死、因不稳定型心绞痛或心力衰竭住院以及冠状动脉血运重建手术的实施。最后进行统计学分析。
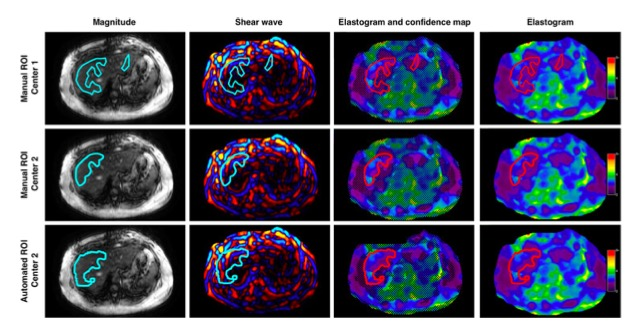
本项研究中的患者平均年龄为 62 岁,49.6% 为男性。在 67,273 名既往无心血管疾病的患者中,9,112 名(13.5%)在 3 年的中位随访期间经历了 MACE。在单变量分析中,FIB-4 ≥2.67是总体 MACE 的显着预测因子( [HR] 1.82,95%CI:1.63-2.04,P<0.001)。在调整已确定的心血管危险因素后,FIB-4≥2.67 仍然是总体 MACE 的最强预测因子(HR [aHR] 1.80,95% CI:1.61-2.02,P< 0.001)并且始终与心肌梗死相关(aHR 1.46, 95% CI:1.25–1.70, P< 0.001),也与因不稳定型心绞痛住院(aHR 1.24, 95% CI:1.03–1.49, P= 0.025)、因心力衰竭住院 (aHR 2.09, 95% CI:1.86–2.35, P< 0.001)、冠状动脉搭桥术 (aHR 1.65, 95% CI:1.26–2.17, P< 0.001) 和经皮冠状动脉介入治疗 (aHR 1.72, 95% CI:1.21–2.45, P= 0.003)相关。
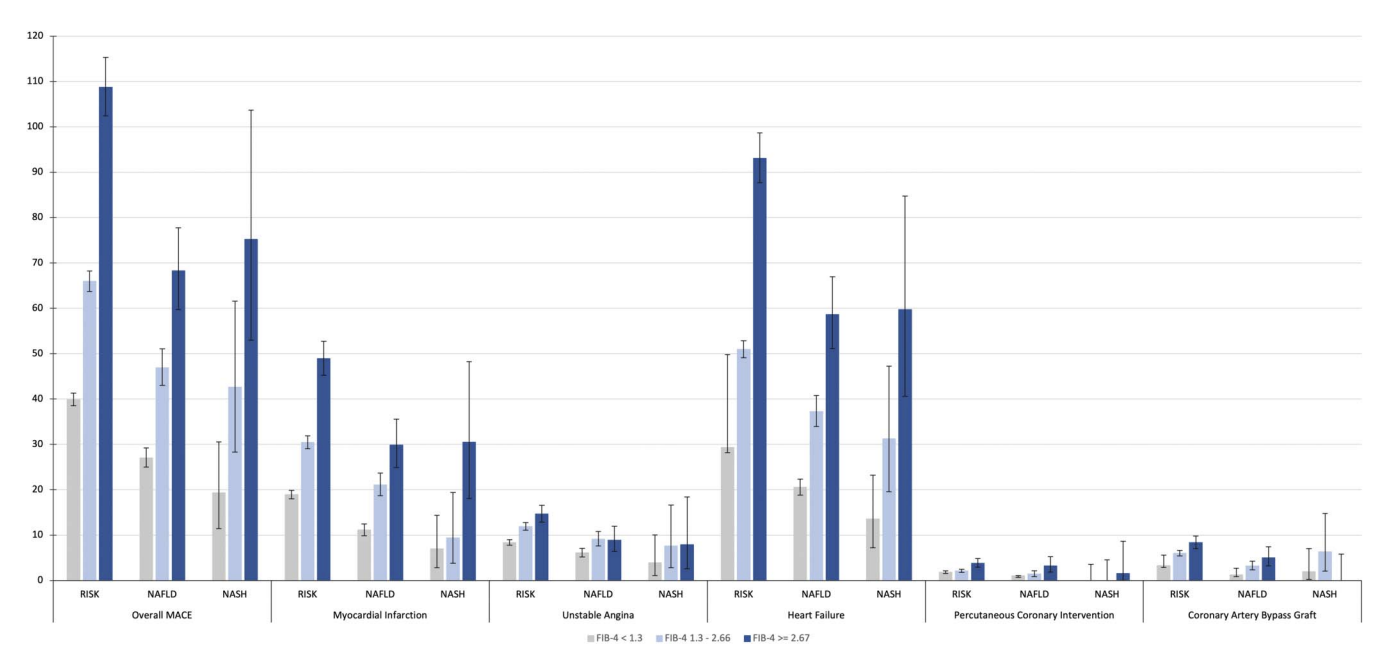
图:Fibrosis-4指数在不同肝病中的表现
本项研究结果证实在一个大型的、真实世界的 NAFLD、NASH 或 NASH 风险患者队列中,FIB-4 评分是 MACE 的最强独立预测因子。
原始出处:
Vieira Barbosa. Et al. Fibrosis-4 Index Can Independently Predict Major Adverse Cardiovascular Events in Nonalcoholic Fatty Liver Disease. The American Journal of Gastroenterology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#酒精性脂肪肝#
87
#AJG#
92
#非酒精性#
82
#发生率#
69
#酒精性#
78
#ROS#
67
#心血管不良事件#
70
#Fibrosis#
90