JCO:口服避孕药不降低BRCA1/2突变携带者的卵巢癌及乳腺癌风险
2013-10-31 ecoliDH5 丁香园
口服避孕药与卵巢癌关系 研究要点: 本研究针对因BRCA1/2突变或有较强家族史而存在卵巢癌或乳腺癌风险增加的女性,评价了口服避孕药对两种肿瘤的相关风险;针对BRCA1/2突变携带者总体的荟萃分析表明,口服避孕药与卵巢癌间存在负向关联,但与乳腺癌间并无统计学意义的显著关联;BRCA1及BRCA2突变也有类似结果。 在2013年10月21日在线出版的《临床肿瘤学杂志》(Jour
口服避孕药与卵巢癌关系
研究要点:
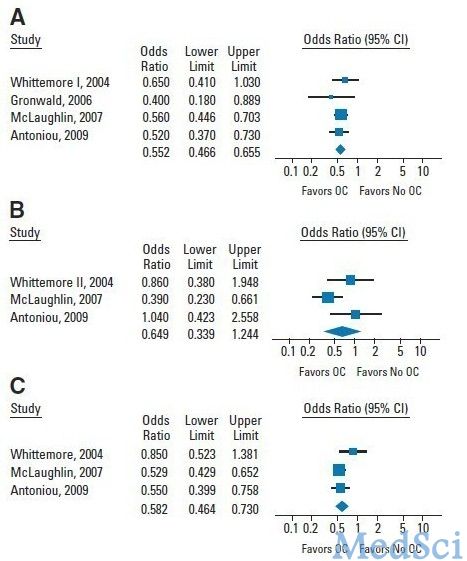
本研究针对因BRCA1/2突变或有较强家族史而存在卵巢癌或乳腺癌风险增加的女性,评价了口服避孕药对两种肿瘤的相关风险;针对BRCA1/2突变携带者总体的荟萃分析表明,口服避孕药与卵巢癌间存在负向关联,但与乳腺癌间并无统计学意义的显著关联;BRCA1及BRCA2突变也有类似结果。
在2013年10月21日在线出版的《临床肿瘤学杂志》(Journal of Clinical Oncology)上,发表了美国杜克大学医学院Patricia G. Moorman博士等人的一项研究结果,该研究针对因BRCA1/2突变或有较强家族史而存在卵巢癌或乳腺癌风险增加的女性,评价了口服避孕药(OC)对两种肿瘤的相关风险。该分析研究表明,对于BRCA1或BRCA2突变携带者,OC用药与卵巢癌和乳腺癌间的关联与既往报告的一般人群类似。【原文下载】
作者对PubMed、Embase、Cochrane系统评价数据库及ClinicalTrials.gov进行了搜索,这些出版于2000年至2012年间的相关研究,针对BRCA1/2突变携带者或有乳腺癌或卵巢癌家族史的女性,评价了OC用药与两种肿瘤间的关系。
该文作者在6,476份独立引文中,共甄别出6项旨在考查BRCA1/2突变携带者卵巢癌风险的研究,8项旨在考查BRCA1/2突变携带者乳腺癌风险的研究。针对BRCA1/2突变携带者总体的荟萃分析表明,OC用药与卵巢癌间存在负向关联,但与乳腺癌间并无统计学意义的显著关联。对BRCA1及BRCA2突变进行分别考查后也得到类似结论。由于数据有限,作者未进行考查用药时长或用药时间的荟萃分析。对于有卵巢癌或乳腺癌家族史的女性,共甄别到4项考查卵巢癌风险的研究,3项考查乳腺癌风险的研究,但由于研究间存在差异,无法对相关数据进行联合荟萃分析,因此不能得出总体趋势结论。
研究背景:
尽管卵巢癌仅为2012年美国女性第九大常见确诊肿瘤(~22,000例),但却为第五大致死癌症类型(~15,000死亡病例)。卵巢癌的较高死亡率由肿瘤分期情况所致,多数病例在确诊时即为III期或IV期病情。尽管早期筛查策略概念诱人,但目前为止尚没有筛查策略得到有效认证。
一般人群终生的卵巢癌风险为1.4%。而对于携带BRCA1或BRCA2突变的女性,BRCA1突变携带者在70岁时的卵巢癌患病风险估计达39%,BRCA2突变携带者则为11%。尽管BRCA1及BRCA2突变携带者占总人口的比例较低(分别为0.12%及0.2%),但由于突变携带者卵巢癌风险较高,因此有必要对可能影响发病的因素进行强化认识。
对于已知存在基因突变或家族史的女性进行初级预防颇具吸引力。对BRCA1/2突变携带者进行双侧输卵管-卵巢切除可分别降低80%及50%的卵巢癌与乳腺癌风险。尽管健康-经济决策模型表明,BRCA携带者接受该手术治疗可达到有效及经济有效的目的,但该手术可导致过早绝经,并伴有包括心血管疾病风险增加在内的潜在危害。因此,部分高风险女性倾向于选择侵犯性较低、可保留卵巢与生育功能的手段进行预防。
一个可能降低遗传风险较高女性卵巢癌发病风险的手段是通过口服避孕药(OC)进行化学药物预防。对于一般人群,OC用药与约30%的卵巢癌发病率降低有关,随着用药期增加,相关风险降低更多。假如OC用药也可降低高风险女性的卵巢癌发病率,那么此类药物将可作为未完成生育或希望避免手术女性的一个可行预防策略。尽管如此,也必须对OC的急性作用(如血栓)及长期风险(如乳腺癌)进行考量。
在一般人群中,乳腺癌风险增加与OC用药史之间存在轻度关联(风险比[OR]≈1.08),目前用药或近期用药者的风险较高。OC用药与卵巢癌间的负向关联远高于其与乳腺癌间的正向关联;然而,乳腺癌发病率较高,且乳腺癌BRCA1/2突变外显度高于卵巢癌。因此,必须就OC的化学药物预防效果与可能的乳腺癌风险增加进行权衡。
在美国医疗保健研究与质量局(AHRQ)与美国疾病预防控制中心(CDC)发起的系统性考察中,本文作者曾对OC用药与降低卵巢癌发病率的潜在获益与风险进行了评价。本文则针对携带BRCA1或BRCA2突变以及有两种肿瘤家族史的特定女性群体,报告了OC用药与卵巢癌和乳腺癌风险间的关联。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了,谢谢作者分享!
138
有理有据,很好学
253
#癌风险#
75
#乳腺癌风险#
118
与以前的认知不一样哈,感谢
195
#JCO#
54
#携带者#
98
#BRCA1#
83
#BRCA1/2#
94
#口服避孕药#
66