BMJ:延迟二次除颤治疗持续性VT/VF可增加患者的住院率
2016-04-08 MedSci MedSci原创
来自美国东部的一个卫生保健系统描述了第一和第二尝试除颤之间的时间间隔的趋势以及与此时间间隔与因持续性室性心动过速或心室颤动(VT / VF)而住院的患者结局之间的关系。
来自美国东部的一个卫生保健系统描述了第一和第二尝试除颤之间的时间间隔的趋势以及与此时间间隔与因持续性室性心动过速或心室颤动(VT / VF)而住院的患者结局之间的关系。
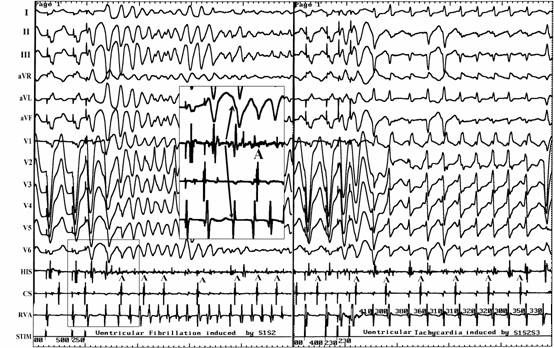
该研究采用回顾性队列研究,分析了2004-2012年参与复苏准则依循登记表的172家美国医院。纳入了在接受第一次持续3分钟除颤后接受第二次除颤尝试性治疗持续性VT / VF的成人患者。二次除颤尝试分为早期(第一次喝第二次除颤的时间间隔长达一分钟)或延迟(时间间隔超过一分钟)。主要研究结果为患者的出院生存率。
结果发现,2733名持续性VT / VF患者在接受第一次除颤尝试后,其中1121名(41%)患者接受延期二次除颤尝试。延迟二次除颤治疗持续VT / VF从2004年的26%增加至2012年的57%。未校正前,与早期二次除颤相比,延迟二次除颤的结局较差(57.4% VS. 62.5%自主循环恢复,38.4% VS. 43.6%存活24小时,和24.7% VS. 30.8%存活出院)。校正风险后,延迟二次除颤与患者存活出院之间并无关联。
总而言之,自2004年以来,因延迟二次除颤治疗持续性VT / VF的使用使得患者的住院率翻了一番。延迟二次除颤并不能改善患者的生存率。
原始出处:
Steven M Bradley, Wenhui Liu, et al., Defibrillation time intervals and outcomes of cardiac arrest in hospital: retrospective cohort study from Get With The Guidelines-Resuscitation registry. BMJ 2016; 353 doi: http://dx.doi.org/10.1136/bmj.i1653 (Published 06 April 2016)Cite this as: BMJ 2016;353:i1653.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#持续性#
61
#BMJ#
59
文章不错
152
值得关注
176
#除颤#
65
血供是王道
130
很有指导意义,迅速终止恶性心律失常,改善症状,缩短住院率。
200