吃抗血栓药,你的基因“配合”吗?
2015-06-30 田埂Geneis 果壳网
为了控制疾病,如今许多人需要长期不间断地服用药物,最常见的莫过于降压药和抗血栓药(抗凝血药)。我的母亲每天服用降压药,已经超过二十年。而父亲七年前中风、今年又发生第二次中风,因此每天必须服用阿司匹林和华法林。然而,这两种广泛使用的抗凝血药物,在我父亲身上却效果不太明显。查阅过许多药物与遗传的相关文献后,我发现,还有其他患者曾遇过同样麻烦,而原因可能是“基因不配合”。阿司匹林(Aspirin):
为了控制疾病,如今许多人需要长期不间断地服用药物,最常见的莫过于降压药和抗血栓药(抗凝血药)。我的母亲每天服用降压药,已经超过二十年。而父亲七年前中风、今年又发生第二次中风,因此每天必须服用阿司匹林和华法林。
然而,这两种广泛使用的抗凝血药物,在我父亲身上却效果不太明显。查阅过许多药物与遗传的相关文献后,我发现,还有其他患者曾遇过同样麻烦,而原因可能是“基因不配合”。
阿司匹林(Aspirin):传奇也会遭遇“抵抗”
先从“神药”阿司匹林说起。
自1897年问世以来,阿司匹林的传奇就从未完结。若以每片药含50 mg阿司匹林计算,全球每年消耗的阿司匹林超过1000亿片,无怪乎它在1950年就以“销量最高的药物”入选了吉尼斯世界纪录。2004年,英国人杰弗里斯(Diarmuid Jeffreys)把阿司匹林的历史写成了一本《阿司匹林传奇》。直到今天,人们对它的兴趣丝毫没有减弱,每年都有相关科研论文发表。
阿司匹林最初并不是抗血栓药,而是对付头疼脑热的居家药品。最早的阿司匹林是从柳树皮中提取出来的。公元前400年,希腊名医希波克拉底(Hippocrates)就记述了柳树皮的医学价值。但阿司匹林的活性成分——乙酰水杨酸是在1853年才合成成功。到了1897年,拜耳的化学家、海洛因“止咳药”的合成者,菲力克斯•霍夫曼(Felix Hoffmann)终于合成出一种稳定的乙酰水杨酸。又过了不到两年,拜耳就推出了命名为“阿司匹林”的止痛药。
Aspirin这个名字,是由乙酰基的首写字母“A”与绣线菊类植物(水杨苷成分的来源)一词中的“Spir”组合而成,末尾加上了一个当时药物的常见后缀“in”。
从药理上说,阿司匹林能够阻止血小板黏结形成阻塞,因此可以预防心脑血管疾病,对于有心脑血管家族病史的老年人,以及糖尿病患者尤其有效。
作为预防和治疗动脉血栓性疾病类疾病的基础药物,阿司匹林可以称得上是“活人无数”。一项荟萃分析表明,阿司匹林抗血小板治疗使非致命性心肌梗死减少1⁄3,非致命性中风减少 1⁄4,血管疾病病死率减少1⁄6。
然而, 阿司匹林并非对所有血栓患者都有效,部分患者不能从中获益,即使服用阿司匹林也不能抑制血小板聚集、无法预防血栓形成。有研究报道称,5%-40%的人存在阿司匹林抵抗(AR)。
什么造成了这种“抵抗”?有些研究认为是吸烟、糖尿病、高血脂等因素削弱了阿司匹林的疗效,同时也有研究提示,要预测阿司匹林抗血小板效应的个体差异,最重要的因素是遗传背景差异。
阿司匹林之所以能抑制血小板聚集,目前明确的主要机制是通过抑制一个叫环氧合酶(COX)的蛋白活性来实现的。目前已知有三个COX同功酶:COX-1、COX-2和COX-3。COX-1被认为是种有益的酶,存在于大多数哺乳动物细胞中,而COX-2为诱导酶,其功能是活化巨噬细胞或其他细胞,充斥于炎症组织。关于COX-3的研究则较少。
当身体组织受到某种刺激如外伤、感染,就会激活COX。COX能催化合成各种前列腺素——别以为只有男性有前列腺素,实际上前列腺素广泛存在于人体的各种组织中,是炎症反应的关键。阿司匹林能抑制COX,也就能抑制前列腺素,从而抑制炎症和疼痛,起到消炎止痛的作用。

阿司匹林和布洛芬都能抑制COX蛋白 图片来源: circres.ahajournals.org
问题就出在COX基因身上。
在基因组水平上,常常会出现单个核苷酸的变异。比如说,同一个位点上,一群人是A,另一群人是G。这叫单核苷酸多态性(single nucleotide polymorphism,SNP),是人类可遗传的变异中最常见的一种,占所有已知多态性的90%以上。
一个核苷酸看上去似乎微不足道。但研究却表明,COX-1基因多态性可能妨碍阿司匹林对其乙酰化,影响其作用效果。另一项研究发现,汉族人COX-1基因-1676A>G位点的单核苷酸多态性,与阿司匹林抵抗有强烈的相关性,该基因型的患者更容易发生阿司匹林抵抗。
另外,阿司匹林对COX-1的抑制作用比对COX-2的抑制作用强170倍。也就是说,阿司匹林对COX-2要无能为力得多。一般来说,COX-2在正常组织细胞中极少或不表达。但在一些病理条件下,由于各种内外环境的刺激,可使COX-2过度表达。还有研究发现,突变型等位基因-765G>C位点rs20417的携带者COX-2会过度表达,这是阿司匹林疗效不佳的原因之一。
COX-3目前研究不多,但不难想象,其上的突变或多态性,也将影响阿司匹林的使用效果。
华法林(Warfarin):先检测基因再服药
比起阿司匹林最初“抗炎止痛”的定位,另一种抗凝血药的出身听起来更吓人。华法林早在1948年就成了“灭鼠灵”,虽然已经有其它更有效的鼠药开发出来,但华法林至今依然是灭鼠的奇方。
华法林是一种抗凝血药物,在阻止血栓形成和血栓栓塞病治疗中使用,用于防治血液凝固和凝块在血管内的迁移。20世纪50年代,华法林在对抗血栓形成和防止血栓栓塞上的有效性和安全性被证实。1954年,华法林被批准上市,并沿用至今。如今,华法林是北美使用最为广泛的口服抗凝药。
华法林药效明显,但缺点也不少,比如会跟很多药物发生相互作用,甚至连富含维生素K1的绿叶食物都可能降低药效,再加上每个人的个体差异,就导致华法林的剂量特别难以掌控,吃少了没用,吃多了出事。所以华法林需要过通过血液测试的国际标准化比值(INR)确保安全服用剂量,高于INR可能有流血风险,低于INR可能有血栓形成风险。
近年的临床观察发现,虽然具有相同症状,但是不同病人对华法林使用的个体差异很大,而这些差异跟病人本身的基因背景有直接的关系。
为此,美国FDA在2010年2月修改了华法林的药物说明书,因为剂量的基因特异性,建议在开具华法林处方前对CYP2C9、VKORC1进行基因检测,针对不同的基因类型进行药物剂量调整。
CYP2C9基因编码的蛋白,负责代谢80-85%的左旋(S型)华法林,S-华法林被其代谢后就更容易被排出体外。这种蛋白从属的细胞色素P450酶家族,负责氧化外源性和内源性化合物,也是体内药物代谢的主要酶系。在肝脏的微粒体中, CYP2C9能代谢超过100种治疗性药物。除了华法林以外,还有治疗惊厥和癫痫的苯妥英(Phenytoin),以及常规处方药如醋硝香豆素、甲苯磺丁脲、格列吡嗪氯沙坦和一些非甾体类抗炎药。而肝外的CYP2C9则代谢一些重要的内源性化合物如花生四烯酸、5-羟色胺和亚油酸等。
至于VKORC1则是华法林作用的对象,它的全名叫“维生素K环氧化物还原酶复合物亚单位1”基因。维生素K是凝血所必须的,但需要经过酶的激活。而VKORC1基因编码的蛋白就负责激活维生素K。如果VKORC1基因发生突变,那么维生素K就无法活化,从而导致缺乏维生素K依赖性凝血因子,进而阻止凝血。
从药理上说,华法林作用的靶点正是VKORC1编码的蛋白,华法林通过影响VKORC1蛋白来抑制维生素K,从而干扰维生素K依赖性凝血因子II、VII、IX、X的羧化,使这些凝血因子无法活化,仅停留在前体阶段,从而达到抗凝血的目的。不过,不同人制造的VKORC1蛋白活性有差异,这也就导致了华法林的剂量变得因人而异。
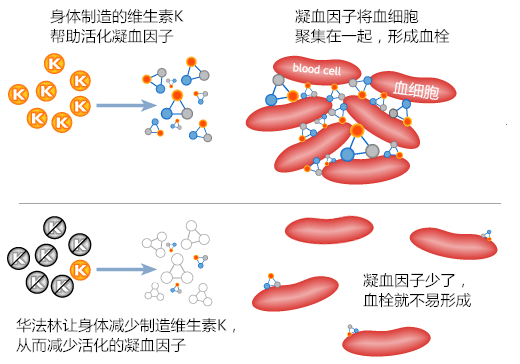
华法林是怎么防止血栓形成的 图片来源:www.emedicalguild.com
最新一版的FDA目录,还增加了PROS、PROC两个基因作为华法林警告和预警的范围,因为这两个基因也参与了凝血的过程,这两个基因编码的是血浆里存在的维生素K依赖性的蛋白。它们如果基因突变会增加形成血栓的倾向,华法林的使用也必须有所不同。
波立维(Plavix):一场法庭争端的主角
波立维又名氯吡格雷,同样是一种非常畅销的抗凝血药物,适用于中风、心肌梗死和外周动脉疾病。从药理学上说,波立维属于二磷酶腺苷(ADP)受体拮抗剂,通过阻止ADP与它的血小板受体结合,来抑制血小板聚集。
关于波立维有一个著名的诉讼,就是2014年3月19日的夏威夷岛民控告药厂百时美施贵宝公司(Bristol-Myers Squibb)和赛诺菲-安万特(Sanofi-Aventis)隐瞒“波立维”对夏威夷岛民无效的诉讼案。
按照药价计算,波立维比阿司匹林要贵100倍,但很多岛民因为看到药品宣传抗凝血效果好于阿司匹林,而用波立维替换了阿司匹林。
然而,由于38-79%的太平洋岛民和40-50%的东亚人遗传易感性低, “波立维”在许多东亚和太平洋岛居民身体中代谢不足,因此无法起效,阿司匹林其实可以保护他们不发生血栓,波立维却并不可以。
但药企自1998年开始就故意隐瞒了这一信息,造成大量患者滥用该药物,增加了经济负担,同时将病人置于危险之中。药厂甚至还隐瞒了一件事,波立维的有效性可以通过简单的CYP2C19基因(rs4244285)检测即可明确判断。
之前说过,CYP2C19编码的蛋白能代谢药物,一般来说,代谢的结果是使药物更容易排出体外,降低药物的效力,但波立维偏偏不是这样,波立维本身是“无活性前体”,要被代谢后才起效,因此,有些人的CYP2C19基因型属于“慢代谢者”,他们服用推荐剂量的波立维后,其活性代谢物的血药浓度就不如“正常代谢者”那么高,不能有效地抑制血小板聚集,从而出现“氯吡格雷抵抗”。
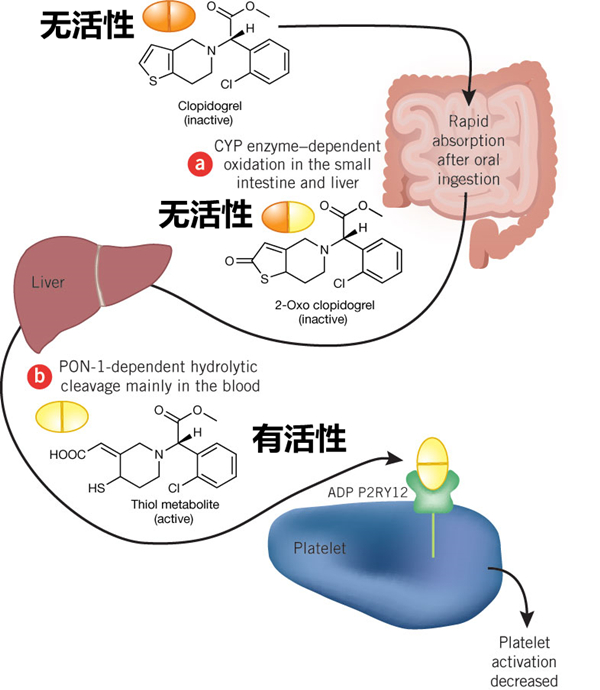
波立维要经肝脏代谢后才有活性 图片来源:nature.com
基因与药物的关系,以前虽被忽略,但正在逐步被人们认识和理解。同一种药物,对于不同的人来说,有效性是不同的,这种不同不只表现为“有效”或者“无效”,还可能表现为“副作用”的强弱,还有药物在身体里停留的时间长短,以及不同药物是否可以一起吃。通过基因的表达和单核苷酸多态性,我们可以确认有无遗传性或获得性的基因变化,这种变化又会怎样影响病人对药物的吸收、分布、代谢和排泄,这,就是所谓的药物基因组学。
如今,根据美国食品和药物管理局(FDA)规定,166种药物对应靶点、65种药物在使用之前要进行基因检测。前文提到的三种被广泛使用的抗凝血药物,其实都可以通过基因检测来确定其有效性,特别是华法林和波立维,证据十分明显,长期服用这两种药物的人,强烈推荐进行基因检测,如果疗效可能不佳,就需要与临床医生商量,针对个人具体情况决定到底是更改剂量,还是换个药物。
对于美国FDA审批过的其它与基因关系明确的药物,也建议大家在用药以前,进行相应的基因检测,以确定服用该药物的有效性和或合理剂量,如此,才是真正的个体化用药和精准治疗。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抗血栓药#
72
122
119
123
169
为了积分!
140
为了积分!
122
为了积分!
160
为了积分!
103
看看
122
#抗血栓#
58
理论不断被质疑,才有新发现
110