CSCO 2016:软组织肉瘤的放疗研究一览
2016-09-26 MedSci MedSci原创
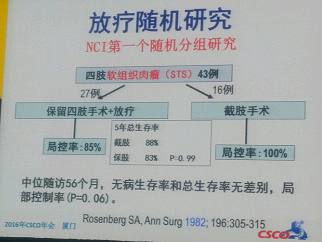
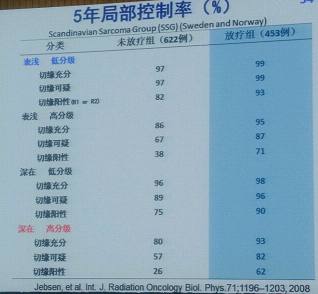
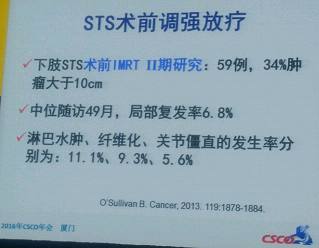
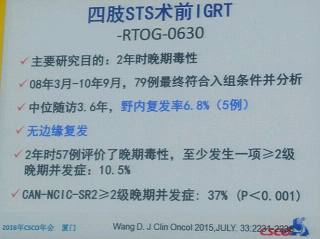
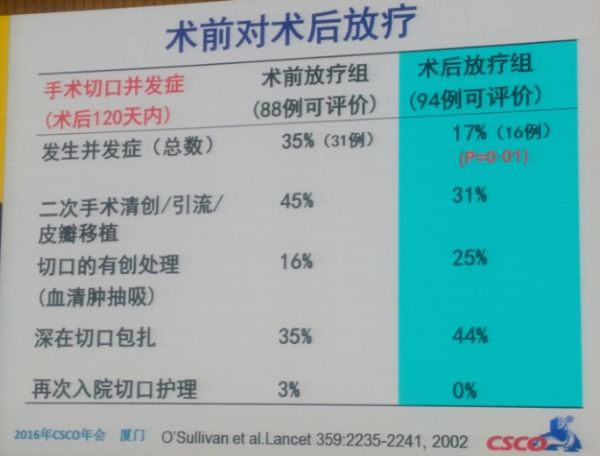
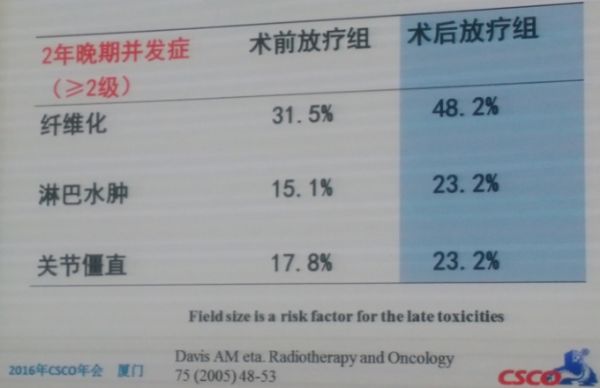
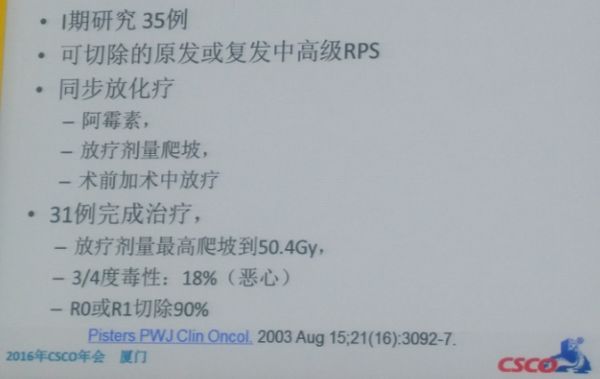
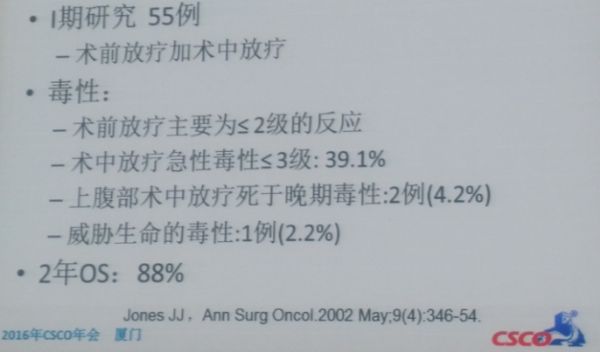
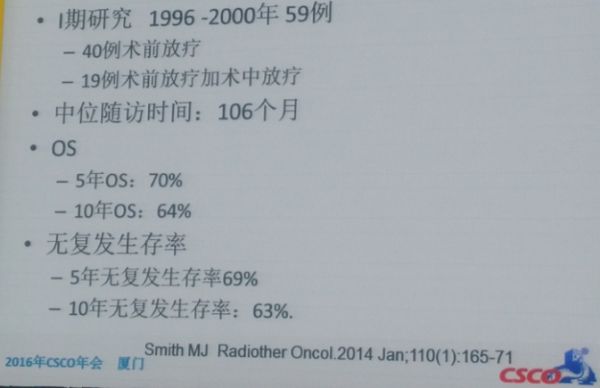
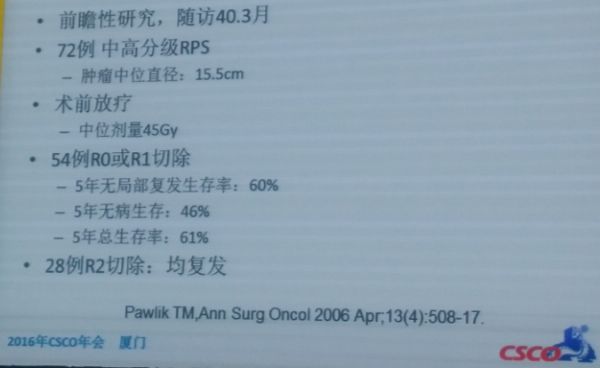
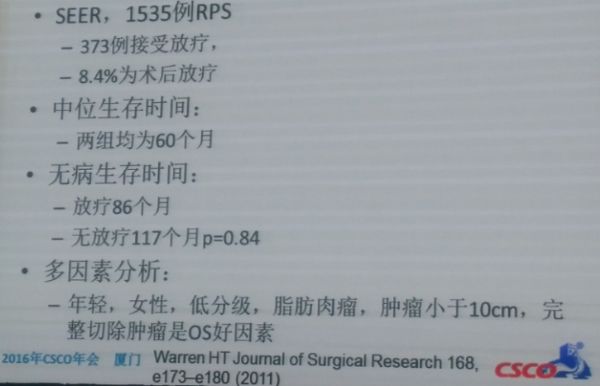
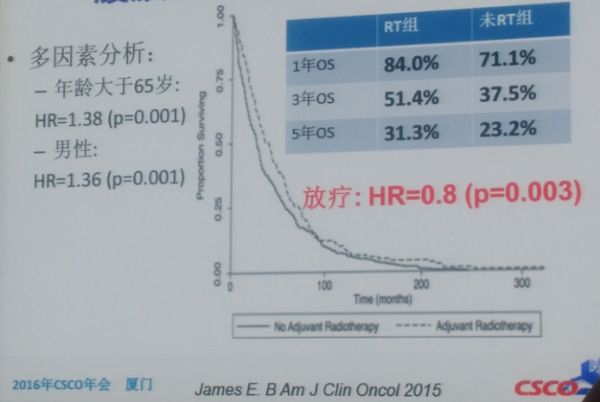
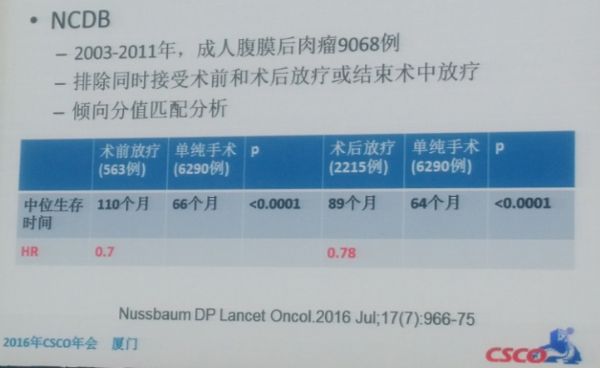
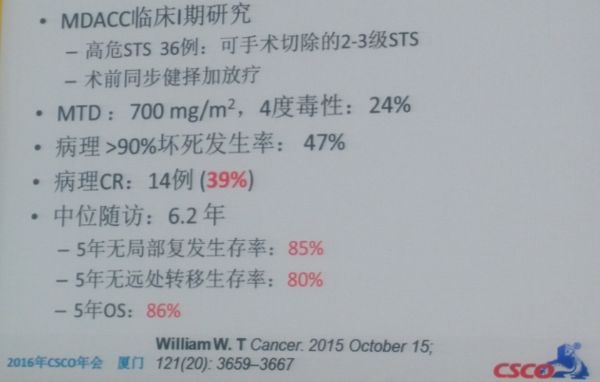
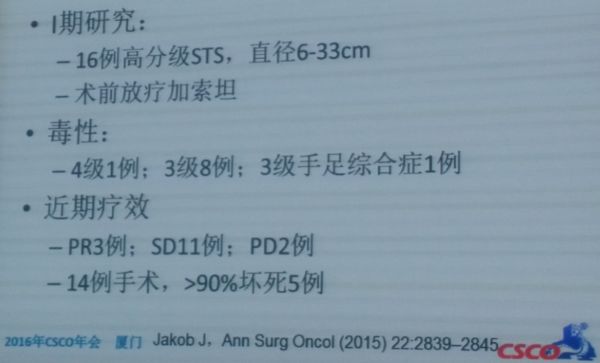
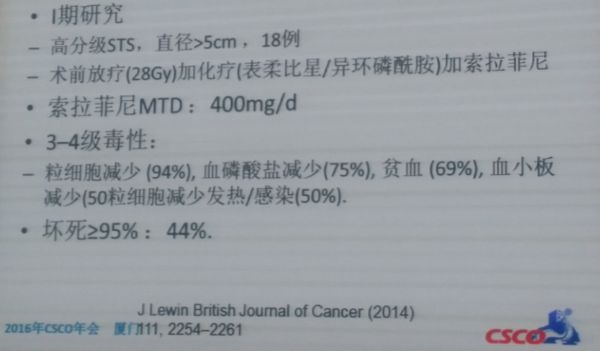
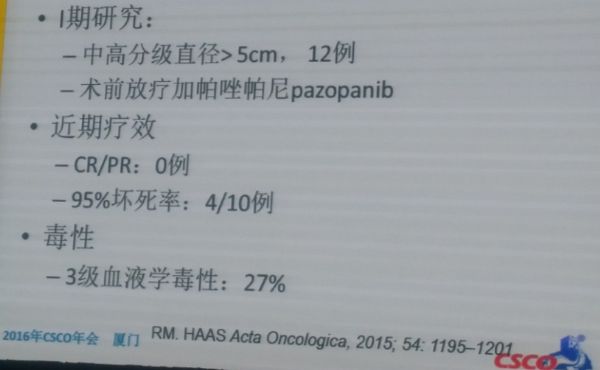
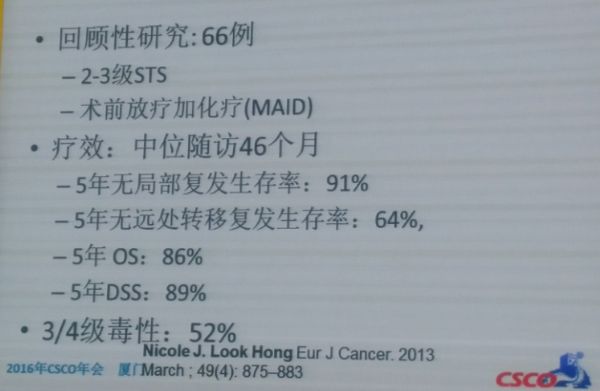
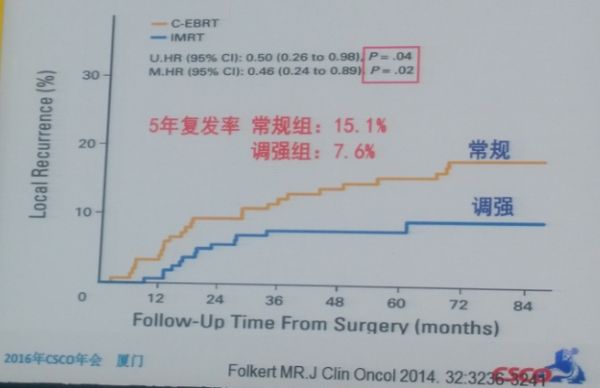
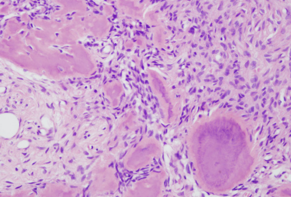
2016年9月22日-24日,第19届全国临床肿瘤学大会暨2016年CSCO学术年会在福建厦门国际会议中心举行。在本届CSCO中,来自中国医学科学院附属肿瘤医院放疗科的房辉和王维虎老师带来了题为《软组织肉瘤的放疗》的精彩报告,下面是梅斯医学小编对其内容的整理:一、放疗的证据最早刊发在1982年Ann surg上2个放疗的随机研究证明了放疗治疗的可取,如下图所示:另,1996年发表在JCO上的一项放
2016年9月22日-24日,第19届全国临床肿瘤学大会暨2016年CSCO学术年会在福建厦门国际会议中心举行。在本届CSCO中,来自中国医学科学院附属肿瘤医院放疗科的房辉和王维虎老师带来了题为《软组织肉瘤的放疗》的精彩报告,下面是梅斯医学小编对其内容的整理:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















谢谢分享,csco
91
#软组织#
64
非常值得学习,要重视
126
继续关注!
88
谢谢分享!
119
学习了,赞一个~
103