Am J Resp Crit Care:鼻咽部微生物和代谢组学与细支气管炎的严重程度相关性分析!
2017-05-22 xing.T MedSci原创
由此可见,多组学分析不仅验证了采用代谢组学的方法来确定细支气管炎严重程度的能力,而且与细支气管炎病理机制中的微生物和宿主之间存在相互关系。
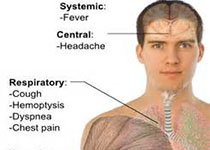
细支气管炎是婴幼儿最常见的下呼吸道感染,但仍不清楚哪些细支气管炎婴幼儿会发生严重的疾病。此外,尽管新兴的证据表明细支气管炎的严重程度与上呼吸道微生物相关,但很少有将气道微生物和宿主对疾病严重程度反应联系在一起的机制。近日,呼吸内科以及重症医学领域权威杂志Am J Resp Crit Care上发表了一篇研究文章,研究人员旨在确定鼻咽气道代谢组谱、微生物谱与细支气管炎患儿疾病严重程度之间的相关性。
研究人员对细支气管炎患儿(年龄<1岁)进行了一项多中心前瞻性队列研究。研究人员应用代谢组学和基因组(16S rRNA基因和全基因组鸟枪法测序)的方法将入院24小时内收集到的144份鼻咽气道样品进行分析,并确定了代谢组学和微生物谱,以及与更严重疾病程度之间的相关性,更严重疾病程度定义为使用正压通气(PPV)-即持续气道正压通气和/或气管插管。
研究人员发现鼻咽气道代谢组谱根据细支气管炎的严重程度明显有所不同(P<0.001)。在确定的254个代谢产物中,25个代谢物在预测使用PPV方面显示出了较高的灵敏度(84%)和特异性(86%)。这些代谢物的强度与肺炎链球菌的相对丰度相关。在通路分析中,神经鞘脂类代谢是使用了PPV的婴儿最显著的富集亚通路,相比于那些没有使用PPV的婴儿(P<0.001)。鞘磷脂代谢产物富集与肺炎链球菌的相对丰度呈正相关。
由此可见,多组学分析不仅验证了采用代谢组学的方法来确定细支气管炎严重程度的能力,而且与细支气管炎病理机制中的微生物和宿主之间存在相互关系。
原始出处:
Christopher J Stewart, et al. Associations of Nasopharyngeal Metabolome and Microbiome with Severity Among Infants with Bronchiolitis: A Multi-omic Analysis. AM J RESP CRIT CARE 2017. https://doi.org/10.1164/rccm.201701-0071OC
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#支气管#
65
#微生物#
66
#相关性#
59
#鼻咽部#
71
#细支气管#
70
#细支气管炎#
71
学习了,谢谢分享
99
相关性分析,相关研究,临床观察,疗效分析
91
#代谢组#
84
#相关性分析#
72