同期两篇Science:基因筛查显示家族性高胆固醇血症被低估
2016-12-26 生物探索 生物探索
导读 Science上在12月23日刊登了两篇文章,美国Geisinger-RGC合作进行的第一篇文章发现一种称为家族性高胆固醇血症的致命遗传性疾病,在诊断和治疗都被低估。Geisinger-RGC的被称为DiscovEHR的另一个合作研究描述了第一个50726的成人参与者的基因组测序和分析,来筛查家族性高胆固醇血症。Science上在12月23日刊登了两篇文章,分别是美国Geisinger健
导读 Science上在12月23日刊登了两篇文章,美国Geisinger-RGC合作进行的第一篇文章发现一种称为家族性高胆固醇血症的致命遗传性疾病,在诊断和治疗都被低估。Geisinger-RGC的被称为DiscovEHR的另一个合作研究描述了第一个50726的成人参与者的基因组测序和分析,来筛查家族性高胆固醇血症。
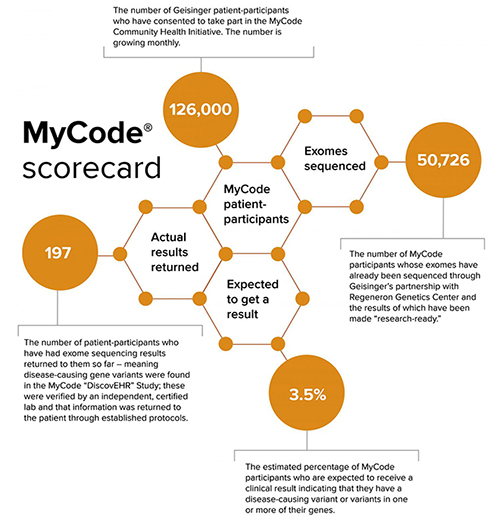
Science上在12月23日刊登了两篇文章,分别是美国Geisinger健康系统与Regeneron遗传学中心(RGC)合作进行的研究,以及Geisinger-RGC的被称为DiscovEHR的合作研究。Geisinger-RGC的第一篇文章“Genetic identification of familial hypercholesterolemia within asingle U.S. health care system”发现一种称为家族性高胆固醇血症的致命遗传性疾病,在诊断和治疗都被低估。DiscovEHR的合作研究“Distribution and clinical impact of functional variants in 50,726 whole-exomesequences from the DiscovEHR study”描述了在Geisinger mycode社区健康倡议所有成员参加的DiscovEHR中第一个50726的成人参与者的基因组测序和分析,来筛查家族性高胆固醇血症。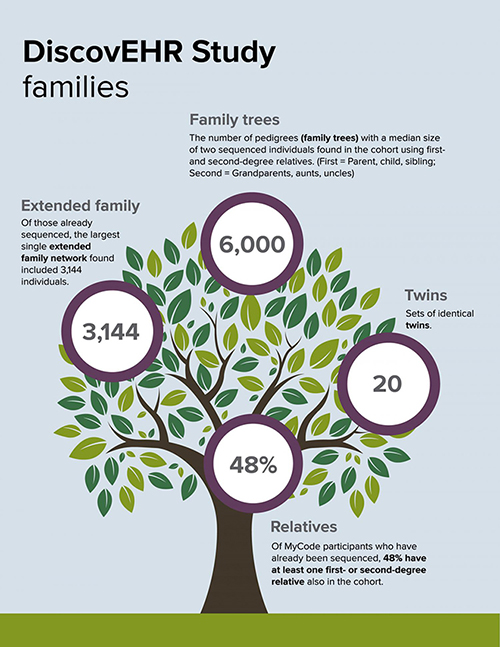
高胆固醇血症被低估
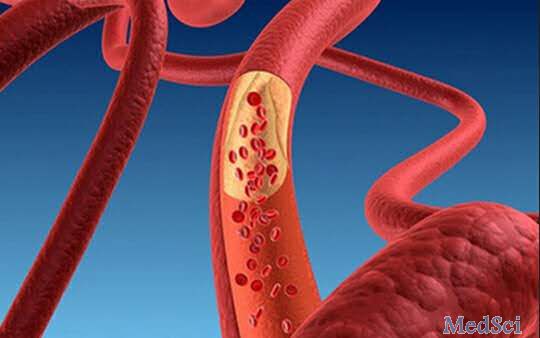
家族性高胆固醇血症的缺陷,使人体无法消除血液中的“坏”胆固醇引起的。这种胆固醇(低密度脂蛋白胆固醇/LDL-C)然后不容易被察觉地积累,即使在非常年轻的人也有可能导致早期死亡的心脏病或中风。传统上,在美国,有早期心脏病和中风家族史的高胆固醇患者被诊断为家族性高胆固醇血症。为家族性高胆固醇血症进行的基因检测,目前在临床上还少见。
在家族性高胆固醇血症的研究中,研究人员在DiscovEHR样本中检测了引起家族性高胆固醇血症的基因变异,并将这些结果与Geisinger电子健康记录中这些患者的医疗史进行比较。
Geisinger临床基因组学的主任Michael F.Murray大夫说:“这项研究揭示了家族性高胆固醇血症是我们预想的两倍那么普遍。对家族性高胆固醇血症的大规模基因检测有助于识别错过的病例。”

在3个家族性高胆固醇血症的基因中,本研究发现每256个人中的1个人会有一个致病突变或变异。研究显示携带家族性高胆固醇血症有害变异的参与者比那些没有的人“坏”的胆固醇要高得多,他们也有着一般和早发性冠心病增加的可能。
RGC遗传学副主任Noura Abul Husn大夫说:“能够将病人的已识别的医疗记录与他们的DNA数据联系起来,是该领域很少有人拥有的一个优势。用RGC的独特的技术和分析资源类配对,让我们能够做出有意义的发现,可能会在今天提前实施精准医学的和在明天开发新的或改进的药物。”
两篇文章的筛查结果
第一篇研究“Genetic identification of familial hypercholesterolemia within asingle U.S. health care system”在LDLR, APOB和PCSK9这三个已被确认导致家族性高胆固醇血症的基因中确定了35个突变或变异。只有24%的携带引起家族性高胆固醇血症的变异的人,在他们的电子健康记录中有家族性高胆固醇血症的确诊。这意味着如果不用基因确认的话,很多这样的病人将未被诊断或治疗。事实上,42%的携带导致家族性高胆固醇血症的变异的人并没有服用他汀类药物来降低胆固醇。在服用他汀类药物的携带导致家族性高胆固醇血症的变异的人中,少于一半达到降低胆固醇的目标。
“Distribution and clinical impact of functional variants in 50,726whole-exome sequences from the DiscovEHR study”则对50726名成人患者的外显子在DiscovEHR的外显子进行了测序,确定约420万罕见的单核苷酸变异和插入/删除事件,其中约176000预计将导致基因功能丧失的。将这些数据与电子病历来源的临床表型相联系,研究人员发现临床协会支持的治疗靶点,其中包括编码降脂药物的靶基因,并发现以前未知的稀有等位基因和与血脂水平和其他血液性状相关的基因。在76个临床可操作的基因中,约3.5%的个人携带有害的变异。
Geisinger执行副总裁兼首席科学官David H.Ledbetter博士说:“Geisinge致力于将这一重要的研究直接转化为对患者更好的护理。我们已经开始尽最大努力在疾病基因筛查中确认人群中发现的病人,并通知参与者个人和他们的医生。”
[1] Noura S. Abul-Husn,et al. Genetic identification of familial hypercholesterolemia within a single U.S. health care system. Science. 23 Dec 2016.
[2] Frederick E. Dewey,et al. Distribution and clinical impact offunctional variants in 50,726 whole-exome sequences from the DiscovEHR study. Science. 23 Dec 2016.
[3] MyCode study finds familia hypercholesterolemia is under diagnosed, under treated. Medicalpress. December 22, 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#基因筛查#
82
#同期#
82
#SCIE#
70
#高胆固醇血症#
0
#家族性#
54