Spine J:抑郁症是腰椎管狭窄手术预后的预测因素
2014-06-11 伊文 丁香园
疼痛和活动受限是腰椎管狭窄(LSS)常见临床症状,可作为判断患者腰椎状况的依据。既往有研究表明,通过 SF-36简明评分可发现腰部术后的患者如果罹患抑郁症则会导致术后功能恢复减慢;很多综述类的文献也证明抑郁症是腰痛独立的预测因素;包括抑郁症在内的心理因素可影响LSS的疼痛等临床症状及其他相关问题的预后。 最近有研究发现LSS患者生存质量下降,与同龄的慢性腰痛的患者相比并发症的发生率增加,这说
疼痛和活动受限是腰椎管狭窄(LSS)常见临床症状,可作为判断患者腰椎状况的依据。既往有研究表明,通过 SF-36简明评分可发现腰部术后的患者如果罹患抑郁症则会导致术后功能恢复减慢;很多综述类的文献也证明抑郁症是腰痛独立的预测因素;包括抑郁症在内的心理因素可影响LSS的疼痛等临床症状及其他相关问题的预后。
最近有研究发现LSS患者生存质量下降,与同龄的慢性腰痛的患者相比并发症的发生率增加,这说明诸如神经性跛行等LSS特异性的症状会加重该类患者的病情,因此抑郁症对于LSS和腰痛患者的影响可能存在差异,但抑郁症对于LSS术后症状严重性的预测是否具有价值尚不清楚。因此Alberta大学康复医学学院的Ashley B等人对此问题进行了系统分析,并发表于最近的The Spine Journal上。
本研究所纳入文献需符合的标准:1.对原始临床数据资料进行报道分析的文献;2.有关抑郁症作为LSS预测因素的相关研究报道,a 明确涉及了评估抑郁症或抑郁症状的研究方法,b 研究对象的诊断包括LSS,c LSS与腰痛鉴别不清的文献需排除;3.纵向研究设计,不包括横断面研究、病例报告、述评、综述、致编辑的信和评论;4. 1980年至2012年5月间发表的英文文献。

作者采用最佳证据综合的方法(Best-evidence synthesis),该研究涵盖了1980年到2012年5月间出版所有相关文献。每篇文献必须符合包括纵向设计在内的纳入标准,所有文献均由两名作者分别对其方法学的治疗进行严格的审核,两名作者评估结果一致的文章方可纳入。
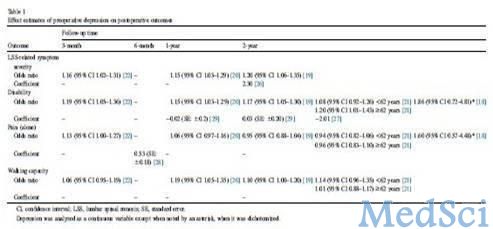
最终有20篇文章符合纳入标准,其中13篇同时被两名作者认为研究方法是科学的。系统分析证据表明术前抑郁症与术后LSS相关临床症状(疼痛、麻木、肌力减弱、失平衡等问题)及活动障碍有关,但抑郁症状和其他症状,活动障碍二者之间的相关性是变化的,从无相关性到中度相关不等。例如随访中发现抑郁评分由63分增长为68分时可使低于中位数的LSS相关症状严重程度评估的优势比翻倍。此外术前抑郁症与术后疼痛及行走能力的相关性变异更大。
在随访的各个阶段均能找到证据支持术前抑郁症是术后LSS相关临床症状严重性和活动障碍独立的预测因素,但对于术后疼痛和行走能力的预测价值尚不十分明确。由于本研究纳入的病例均为手术患者,许多相关文献也没有纳入本研究中,但无论如,对LSS患者诊疗护理时应当充分考虑到抑郁症的影响。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#椎管狭窄#
67
#椎管#
94
#Spine#
68
#预测因素#
61
#腰椎#
58
#腰椎管狭窄#
76
#腰椎管#
67