Nature Communications:新发现的分子对血管炎症具有双重保护作用
2021-04-22 Viho MedSci原创
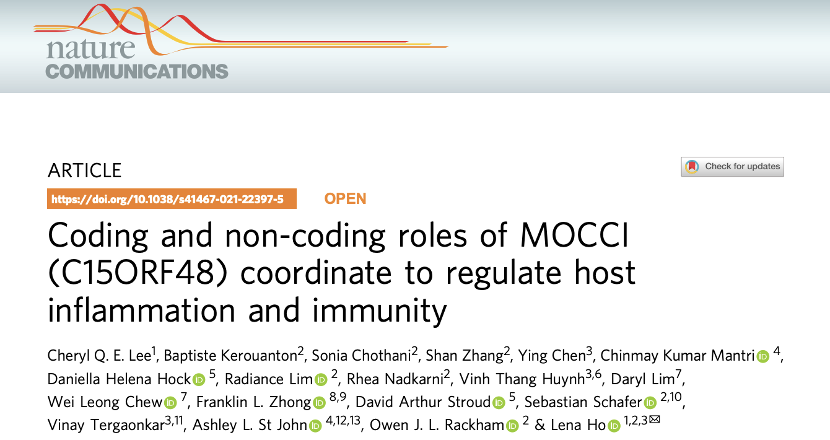
近日,来自美国杜克大学医学院和新加坡科学技术研究机构(A*STAR)的多学科研究小组发现了一种名为MOCCI的新线粒体肽,在调节血管炎在调节血管炎症和免疫方面发挥着重要作用。
血管炎症,可导致组织损伤、动脉粥样硬化和纤维化等心血管疾病。尽管一些治疗方法在临床试验中显示出有希望的结果,但有相当大的副作用,如免疫抑制导致感染的风险增加,而且疗效有限。因此,迫切需要更有效的治疗方法。
fuhg
近日,来自美国杜克大学医学院和新加坡科学技术研究机构(A*STAR)的多学科研究小组发现了一种名为MOCCI的新线粒体肽,在调节血管炎症和免疫方面发挥着重要作用。这项发表在Nature Communications上的研究,揭示了一个基因是如何编码两个分子,在病毒感染后提供双管齐下的保护。
鉴于线粒体酶是由核基因组中的sORFs编码的肽,被导入线粒体,用于线粒体功能的各个层面。在描述参与代谢调节的线粒体-SEPS时,研究人员发现线粒体-SEPS和炎症途径之间存在着意想不到的负相关关系,如扩张型心肌病的人类心脏转录组中的干扰素信号,是一种慢性血管炎症的设置(图1a)。促使研究者设计了一种策略,以发现迄今为止尚未定性的参与调节炎症,特别是血管系统的炎症线粒体-SEPs。
研究人员采用了一种无偏见的蛋白质基因组学策略,基于核糖体谱(Ribo-seq)和RNA测序(RNA-seq),对用IL-1β处理的初级HAECs进行处理(图1b)。随后选择了处理后45分钟、12和24小时来捕捉炎症反应的全过程,包括解决激活的促炎症标志物NF-κB活性、ICAM-1和VCAM-1的下降趋势所示(图1b)。
此外,研究团队还使用来自两个健康男性捐赠者的HAECs,一式三份,以避免捐赠者的特定影响,并进行配对的Ribo-seq与RNA-seq。使用RiboTaper13从遗数据集中识别所有属于基因组中已知共识编码序列(CCDS)区域的表达的ORFs。这些被过滤的ORFs只包括编码小于100个氨基酸的肽,并排除那些与较大蛋白质重叠的ORFs(图1c)。只有那些符合基于已知SEPs参数的质量控制指标的才被保留。
研究分析确定了21个推定的炎症性线粒体-SEPS(i-Mito-SEP)(图1c)。
根据其差异性表达的程度,以及它是否对线粒体动机、基因特征或两者都是阳性的,对每个幸存的候选者进行了分类(图1e)。排名第一的i-Mito-SEP候选者是由C15ORF48基因编码的一个83aa的肽,也叫NMES-1,它在IL-1β处理后显示出最大的上调,并且两种预测方法都预测它是线粒体(图1e)。
此外,还证实了IL-1β处理后Ribo-seq读数增加,表明炎症期间有更多的翻译(图1f)。在整个ORF中也检测到了框内P-位点读数(图1g)。这使得研究者能够区分备用的翻译起始点,并准确地确定SEP的起始点。

人内皮细胞(HAECs)蛋白质组筛选鉴定Mocci为炎症性Mito-SEP(I-Mito-SEP)
整个研究结果发现,MOCCI是复合体IV的一个迄今未知的成分,复合体IV是线粒体中负责产生能量的一系列酶的一部分,称为电子传输链。在炎症期间,MOCCI并入复合物IV以抑制其活性,且这种抑制作用是减少病毒感染后的炎症所必需的。
研究人员还发现,MOCCI是与一种名为miR-147b的微型RNA分子一起制造的。这两个分子由同一基因的不同部分组成。Mocci起源于编码蛋白质的基因序列,而miR-147b则来自非编码区。
MiR-147b分子在发挥抗炎作用的同时,积极阻止病毒复制。这意味着MOCCI和miR-147b协同发挥作用,帮助控制病毒感染和抑制炎症。
这项研究的主要作者Cheryl Lee博士表示,MOCCI实质上改变了细胞中部分能量产生中心的用途,以调节炎症。
研究人员表示,下一步将探索如何开发能够模仿miR147b的抗炎作用的靶向药理疗法,还计划调查MOCCI在结肠炎和牛皮癣等常见慢性炎症性疾病中的作用。
原始出处:
Cheryl Q. E. Lee et al. Coding and non-coding roles of MOCCI (C15ORF48) coordinate to regulate host inflammation and immunity, Nature Communications (2021). DOI: 10.1038/s41467-021-22397-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#新发现#
99
#Nat#
85
#COMMUN#
96
#血管炎#
77
#血管炎症#
92
#Nature Communications#
62
#保护作用#
83