Spine J:腰椎术中静脉用利多卡因可缓解术后疼痛
2014-09-11 orthowhq 丁香园
腰椎椎间盘切除手术的目的是减缓疼痛,但手术本身可导致术后疼痛。绝大多数患者经历术后腰痛,导致术后住院时间延长和恢复正常活动时间延迟。为减轻术后疼痛,不得不使用麻醉药或止痛药,可致并发症,包括谵妄,恶心,呕吐,呼吸抑制等。因此,减少术后使用麻醉药或止痛药就很必要。 利多卡因是众所周知的局麻药,在某些病例具有抗炎和抗缺血效应。另外,术后疼痛与多种机制有关,包括痛觉敏感,炎症,肌肉痉挛,肠道胀气和组织
腰椎椎间盘切除手术的目的是减缓疼痛,但手术本身可导致术后疼痛。绝大多数患者经历术后腰痛,导致术后住院时间延长和恢复正常活动时间延迟。为减轻术后疼痛,不得不使用麻醉药或止痛药,可致并发症,包括谵妄,恶心,呕吐,呼吸抑制等。因此,减少术后使用麻醉药或止痛药就很必要。
利多卡因是众所周知的局麻药,在某些病例具有抗炎和抗缺血效应。另外,术后疼痛与多种机制有关,包括痛觉敏感,炎症,肌肉痉挛,肠道胀气和组织缺血。因此,关于静脉用利多卡因和术后疼痛间的报道常不一致。因此,关于静脉全身应用利多卡因的效应,目前尚不明确。
韩国庆北国立大学医院神经外科的学者,进行了一项双盲随机对照临床试验研究,提示腰椎间盘切除术中静脉全身应用利多卡因可减轻术中痛觉,从而减少阿片类用药和术后疼痛,缩短住院时间,文章于2014年8月发表在Spine J上。
该临床试验研究共纳入51例单节段腰椎椎板切除、间盘切除的病例,麻醉方式为全麻。患者随机分为(以随机程序进行,由独立的统计学家完成)利多卡因组和生理盐水对照组,患者进入手术间,麻醉诱导前,打开信封,其中的卡片提示患者为哪个组。另外,给于利多卡因或生理盐水无标注。
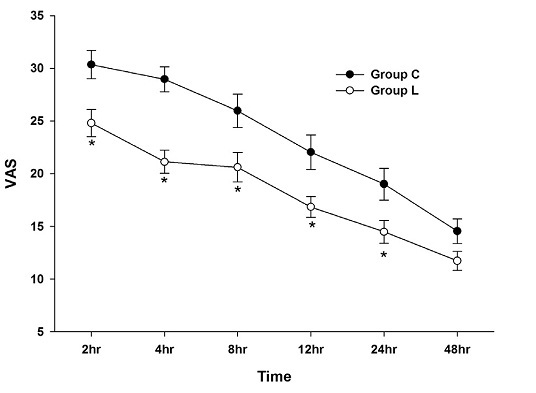
利多卡因组静脉全身应用,剂量为1.5mg/Kg起始量,继以2mg/Kg/h直至手术结束。对照组给于生理盐水为安慰剂。主要评估指标为术后4小时视觉模拟量表(0-100mm)疼痛分值,次要指标包括术后2,8,12,24,48小时视觉模拟量表疼痛分值、芬太尼用量及患者按压镇痛装置按钮的频次。其他指标包括对于疼痛控制和总体过程的满意度,术后恶心和呕吐发生率及住院时间。
结果显示,25例分为利多卡因组,26例分为对照组。利多卡因组的视觉模拟量表疼痛分值和芬太尼用量,在术后各时间点明显低于对照组,除外术后48小时(图1)。利多卡因组的总芬太尼用量,总按压频次,住院天数(短1天),明显低于对照组,而满意度高于对照组。

图1 腰椎术后视觉模拟量表疼痛分值。数值为均数加减标准差。*为统计学显著差异。
以上结果表明,术中全身应用利用卡因可减轻腰椎间盘切除术中的痛觉,因而减少了阿片类药物的用量和术后疼痛,进一步缩短了住院天数。静脉用利多卡因可在术后48小时内减缓疼痛,在24小时内减少芬太尼用量。
本研究为首次临床试验,证实了静脉用利用卡因在腰椎间盘切除术后的功效。其机制为多方面,但防止中枢性疼痛似为其中之一。由损伤区域的疼痛信号由外周A和C纤维传入中枢神经系统,利多卡因阻滞了这些神经元上电压敏感钠离子通道。其他可能的机制为肌肉保护效应,防止缺血再灌注损伤等。
本研究的缺点在于,未检测血浆中利多卡因浓度,未分析术中脊柱肌肉压力。本研究中的病例无合并有其它严重疾病,因而本研究的结果不应用于合并严重疾病的患者。
原始出处
Kim KT1, Cho DC1, Sung JK1, Kim YB2, Kang H3, Song KS4, Choi GJ5.Intraoperative systemic infusion of lidocaine reduces postoperative pain after lumbar surgery: a double-blinded, randomized, placebo-controlled clinical trial.Spine J. 2014 Aug 1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








值得收藏,学习,谢谢分享
106
#Spine#
74
#静脉#
51
#腰椎#
42
#利多卡因#
47