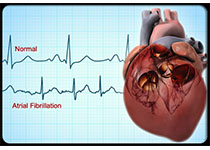
Circulation:子女患先天性心脏病,母亲以后患心血管疾病的长期风险也更高!
2018-06-01 MedSci MedSci原创
背景:先天性心脏病预示家族性心血管疾病的可能性尚未被研究。孕育过先天性心脏病胎儿的女性在以后的生活中患心血管疾病的风险是否会更高?Nathalie Auger等人对此进行研究。方法:本研究队列由1989-2013年间在加拿大魁北克分娩过的1084251位女性组成。研究人员对这些女性的子女是否有心脏缺陷(严重缺陷、非严重缺陷和正常)进行鉴定,并追踪其是否患心血管疾病,随访时间扩展至分娩后25年。研究
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












逆向思维.学习了.
92
很好.开拓了思路.反过来思考
80
开拓了思路
89
#先天性#
60
#长期风险#
79
#血管疾病#
47
一起学习学习
81
学习谢谢分享
92