Blood:Sos1缺陷可缓解致瘤性Kras[G12D]所诱导的骨髓增生性肿瘤
2018-11-02 MedSci MedSci原创
中心点:Sos1介导致瘤性Kras诱导的野生型Nras和Hras超活化。Sos1-/-可减弱Kras[G12D]诱导型MPN,延长Kras[G12D]小鼠的存活期。摘要:研究人员既往发现Kras[G12D]在血液恶性肿瘤中的致癌性比Nras的更强。Xiaona You等研究人员认为Kras[G12D]具有很强的白细胞生成活性,至少部分原因是在于其独特的超激活野生型(WT)Nras和Hras的能力。
Sos1介导致瘤性Kras诱导的野生型Nras和Hras超活化。
Sos1-/-可减弱Kras[G12D]诱导型MPN,延长Kras[G12D]小鼠的存活期。
摘要:
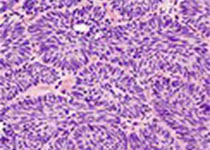
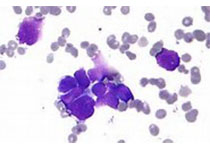
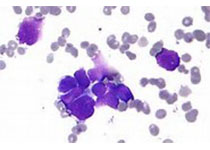
研究人员既往发现Kras[G12D]在血液恶性肿瘤中的致癌性比Nras的更强。Xiaona You等研究人员认为Kras[G12D]具有很强的白细胞生成活性,至少部分原因是在于其独特的超激活野生型(WT)Nras和Hras的能力。现其发现Sos1,鸟嘌呤核苷酸交换因子,参与调控该过程。Sos1在Kras[G12D/+]细胞中过表达,但在Nras[Q61R/+]细胞中无相似情况。在体内,Kras[G12D]蛋白与Sos1形成复合物。在Kras[G12D]细胞中,Sos1缺陷可缓解WT Nras、Hras及其下游ERK信号的超活化。
因此,敲除Sos1可改善致瘤性Kras诱导的骨髓增生性肿瘤(MPN)表型,延长Kras[G12D]小鼠的存活期。相反,在Nras[Q61R/+]细胞中,Sos1对于超激活GM-CSF信号可有可无,敲除Sos1并不影响Nras[Q61R/+]小鼠的MPN表型。
此外,Kras[G12D/+];Sos1-/-小鼠的存活期与采用MEK+JAK抑制剂联合治疗的Kras[G12D/+]小鼠的存活期相差无几。
综上所述,靶向Sos1与致瘤性Kras的相互作用或可提高携带KRAS突变的癌症患者的存活率。
Xiaona You,et al. Unique dependence on Sos1 in KrasG12D-induced leukemogenesis. Blood 2018 :blood-2018-09-874107; doi: https://doi.org/10.1182/blood-2018-09-874107
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#致瘤性#
80
#增生性#
69
#骨髓增生#
99
#骨髓增生性肿瘤#
92
#KRAS#
95
了解一下,谢谢分享!
106