CHEST:非小细胞肺癌I期患者行亚肺叶切除术易复发
2012-12-14 sd3212 丁香园
目前I期非小细胞肺癌患者(NSCLC)接受亚肺叶切除手术(sublobar resection,L-)的比例越来越多。然而,有关这种手术后,患者肿瘤局部复发(LR)的风险及其与手术方式的相关性的资料却很少,尤其是接受亚肺叶切除手术者与接受肺叶切除术(L+)者在这些方面的比较资料更为少见。为了对上述资料加以补充,来自于美国宾夕法尼亚州赫希市佩恩国家癌症研究所的J. Varlotto博士
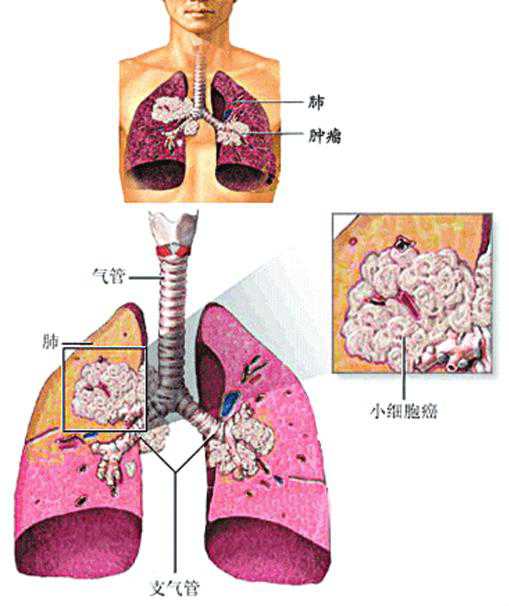
目前I期非小细胞肺癌患者(NSCLC)接受亚肺叶切除手术(sublobar resection,L-)的比例越来越多。然而,有关这种手术后,患者肿瘤局部复发(LR)的风险及其与手术方式的相关性的资料却很少,尤其是接受亚肺叶切除手术者与接受肺叶切除术(L+)者在这些方面的比较资料更为少见。为了对上述资料加以补充,来自于美国宾夕法尼亚州赫希市佩恩国家癌症研究所的J. Varlotto博士及其同事进行了一项研究,研究结果在线发表于2012年11月29日的《胸部》(CHEST)杂志上。作者发现,与接受肺叶切除手术者相比,I期非小细胞肺癌患者接受亚肺叶切除手术后,其肿瘤局部复发的风险增加。这在那些肿瘤分级≥2级或肿瘤大于2厘米的患者中尤其明显。研究者建议,如果准备为I期非小细胞肺癌患者(尤其是那些肿瘤分级≥2级或肿瘤大于2厘米的患者)施行亚肺叶手术切除时,应考虑给予其额外的局部治疗以减少肿瘤局部复发的风险。
该研究的研究对象主要为2000年~2006年间的连续性的非小细胞肺癌患者,其中有93例患者接受了亚肺叶切除手术,318例患者接受了肺叶切除手术。中位随访时间为34个月。
该研究的主要结果为:在亚肺叶切除手术组,患者在手术后第2、3、和5年时的肿瘤局部复发率分别为13%、24%、和40%。肿瘤局部复发的风险与肿瘤分级、肿瘤大小、和肺癌的T分期明显相关。在肿瘤分级≥2级且接受亚肺叶切除手术的患者中,肿瘤局部复发的大致风险为30%(21/69)。在肺叶切除手术组,患者在手术后第2、3、和5年时的肿瘤局部复发率分别为14%、19%、和24%。肿瘤局部复发的风险随着肿瘤的增大、住院时间的延长及糖尿病的存在而显着增加。与肺叶切除手术组相比,亚肺叶切除手术组在支气管残端/缝合线处出现手术失败(肿瘤局部复发)者明显增加(10%对3%,p= 0.04),而同侧肺门及隆突下的手术失败率虽有增加的趋势,但无统计学差异。
该研究结果显示:与接受肺叶切除手术者相比,I期非小细胞肺癌患者接受亚肺叶切除手术后,其肿瘤局部复发的风险增加。这在那些肿瘤分级≥2级或肿瘤大小大于2厘米的患者中尤其明显。研究者建议,如果准备为I期非小细胞肺癌患者(尤其是那些肿瘤分级≥2级或肿瘤大于2厘米的患者)施行亚肺叶手术切除时,应考虑给予其额外的局部治疗以减少肿瘤局部复发的风险。
原始链接:
Donington J, Ferguson M, Mazzone P, Handy J Jr, Schuchert M, Fernando H, Loo B, Lanuti M, de Hoyos A, Detterbeck F, Pennathur A, Howington J, Landreneau R, Silvestri G.American College of Chest Physicians and Society of Thoracic Surgeons Consensus Statement for Evaluation and Management for High-Risk Patients With Stage I Non-small Cell Lung Cancer.Chest. 2012 Dec;142(6):1620-35.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Chest#
57
#亚肺叶#
60
#非小细胞#
82
#EST#
72
#切除术#
73
#肺叶切除#
78