Circulation:IL-6信号遗传缺陷可可降低克隆造血变异个体的心血管风险
2020-01-28 QQY MedSci原创
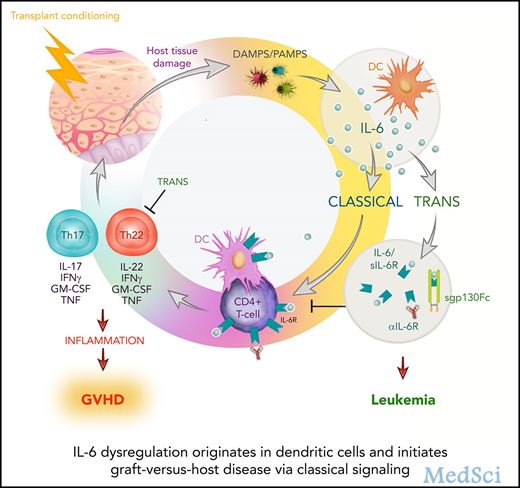
不确定潜能克隆性造血(Clonal hematopoiesis of indeterminate potential,CHIP)是指造血干细胞克隆扩增导致产生获得性白血病突变,如DNMT3A或TET2。在人类中,CHIP与心肌梗死相关。在小鼠中,CHIP可恶化动脉粥样硬化,增加IL-6/IL-1β的表达,引发这样一个推测:IL-6通路拮抗剂或可降低CHIP携带者的心血管疾病(CVD)风险。研究人员
研究人员分析了UK生物库中无CVD的35416位个体的外显子序列,来鉴别携带DNMT3A或TET2 CHIP的个体。研究人员以IL6R p.Asp358Ala编码突变作为IL-6抑制的遗传代理,检测了CHIP状态与CVD事件(心肌梗死、冠脉重建、卒中或死亡)之间的相关性,同时评估其是否受IL6R p.Asp358Ala影响。
共筛选出1079位(3.0%)位携带CHIP的个体,其中432位(1.2%)携带大克隆(等位基因频率>10%)。中位随访6.9年期间,CHIP与CVD事件风险增加相关(风险比[HR] 1.27[95% CI 1.04-1.56],P=0.019),携带大CHIP克隆的个体CVD事件风险增加的更显著(HR 1.59[95% CI 1.21-2.09],P<0.001)。IL6R p.Asp358Ala可降低携带大CHIP克隆个体的CVD事件风险(HR 0.46[95% CI 0.29-0.73],P<0.001),但不影响无CHIP个体的。在9951位独立的受试者中,CHIP状态与心肌梗死的相关性也随着IL6R p.Asp358Ala状态而改变。
CHIP与CVD事件风险增加相关。对于大CHIP克隆的携带者,从基因上减弱IL-6信号可以消除这种风险。
原始出处:
Alexander G. Bick, et al.Genetic Interleukin 6 Signaling Deficiency Attenuates Cardiovascular Risk in Clonal Hematopoiesis.Circulation. 2020;141:124–131
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管风险#
77
#遗传缺陷#
75
#克隆#
60
学习了
119
#IL-6#
69
#变异#
57
#造血#
78
#克隆造血#
51