【一般资料】
患者,男,年龄32岁,于2009年2月于本院牙周科就诊,
【主诉】
牙齿松动,牙龈出血半年。
【现病史】
半年来患者自觉牙齿松动,牙龈出血,自行口服奥硝唑,稍缓解,病情反复发作,时有口腔异味;平均每天刷牙1次,时间不足1min。
【既往史】
自述2型糖尿病9年,口服降糖药,空腹血糖约7.0~8.0mmol/L,
【家族史】
无家族性糖尿病史。
【体格检查】
口腔卫生差,烟斑明显,软垢Ⅰ~Ⅱ度,龈上牙石Ⅰ~Ⅱ度,可探及龈下牙石,牙龈暗红色,龈乳头呈球形,与牙面分离,质地松软,探诊出血(bleedingonprobing,BOP)阳性,部分牙齿牙龈退缩(gingivalrecession,GR)约1mm,
【辅助检查】
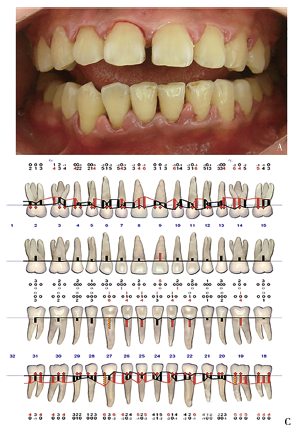
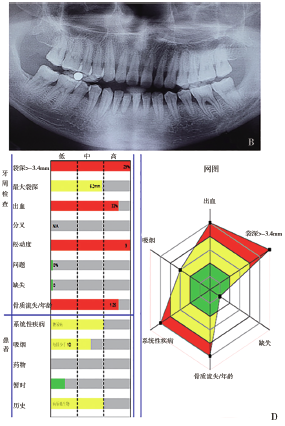
Florida牙周电子探针检查显示:探诊深度(probingdepth,PD)约2~6mm,附着丧失(attachmentloss,AL)约1~4mm,无溢脓,#36颊侧Ⅱ度根分叉病变,#12、#11、#22、#36、#32、#31、#41、#42、#43Ⅰ度松动,覆牙合覆盖基本正常,无龋齿,详见图1A、C。血液检查:空腹血糖7.78mmol/L。X线检查:牙槽嵴顶模糊,牙槽骨水平吸收约为根长1/3,下前牙牙槽骨吸收至根中1/3,#36根分叉牙处槽骨吸收,详见图1B。
【初步诊断】
伴2型糖尿病的慢性牙周炎(中度)。预后判断:中度骨吸收,口腔卫生维护尚可,#36Ⅰ度根分叉病变,Florida危险六因素分析为高风险因素(图1D),血糖控制良好的情况下,预后可/一般。
【治疗】
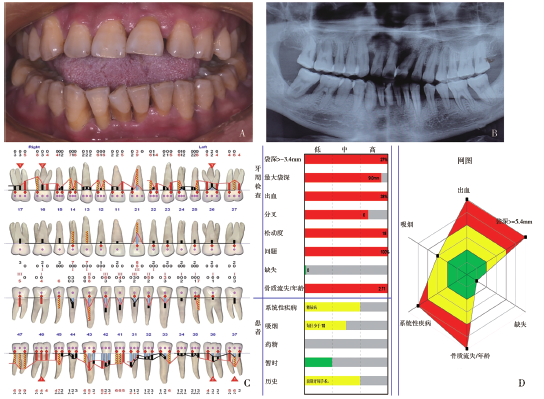
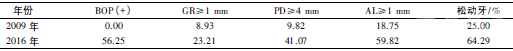
口腔卫生宣教;严格控制血糖浓度;牙周基础治疗;牙周手术治疗;牙周维护治疗。治疗过程:菌斑控制,全口分次进行龈上洁治、龈下刮治、根面平整,菌斑显示,指导患者正确口腔维护方法,治疗期间配合使用抗生素预防感染。该患者于2009年3月基础治疗结束后,患者口腔卫生尚可,软垢Ⅰ度,牙龈红肿消退,无探诊出血,下前牙牙龈退缩约1~2mm,PD≥4mm位点11个,全口菌斑指数40%,详见图2A。此次复诊对残留深袋行二次龈下刮治和根面平整,进行牙周风险因素评估,详见图2B。基础治疗完成后患者失访7年,2016年3月再次复诊,主诉牙周疾病加重,1年前因血糖控制不佳曾住院治疗。临床检查:口腔卫生差,软垢Ⅱ度,龈上牙石Ⅰ度,可探及龈下牙石,牙龈红肿,呈暗紫色,BOP(+),探诊牙周袋,龈缘可见脓液溢出,PD约4~9mm,AL约2~10mm,牙龈退缩2~4mm,牙齿移位,牙间隙明显,#17、#26,#37、#46颊侧Ⅰ度根分叉病变,#16、#36颊侧Ⅱ度根分叉病变,#16、#14、#13、#12、#22、#37、#36、#35、#34、#33、#46松动I度,#32、#43松动Ⅱ度,#21、#31、#41、#42、#47松动Ⅲ度,详见图3A、C。血液检查:空腹血糖13.08mmol/L;X线检查:牙槽嵴顶稍模糊,牙槽骨水平吸收至根中1/3~根尖1/3,#33、#37、#47近中远中牙槽骨角形吸收,其中#21、#31、#41、#42牙槽骨吸收至根尖,#47根尖区低密度影,骨硬板消失,见图3B。预后判断:重度牙槽骨吸收,Ⅰ~Ⅱ度根分叉病变,牙松动达Ⅱ~Ⅲ度,血糖控制不良,Florida危险六因素分析为高风险因素(图3D),预后为差/可疑。治疗计划:仅进行应急处理,建议患者先控制血糖,待血糖控制后尽快进行牙周治疗。根据Lang提出的牙周炎复发评估系统进行复发风险评估:BOP(+)位点<10%,PD≥5mm牙周袋检出1个,暂无牙齿丧失,骨丧失/年龄(BL/Age)为0.5,以上均为低复发危险度;吸烟每日少于10支,为中度复发危险度,全身系统疾病糖尿病为高复发危险度,故评估为中度复发危险度,此时全身危险因素为该患者主要问题。患者2016年复诊时的牙周与2009年初次牙周治疗后牙周检查相比,牙周状况加重明显,牙龈退缩明显,牙周探诊深度普遍增加,深袋比例增加,Ⅱ-Ⅲ度松动牙数明显增加,多位点牙周脓液溢出,详见表1。牙槽骨吸收加重,风险评估为高风险度,此时全身因素及牙周因素均为高危险因素。

小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













天向上好好好好学习天
113
#慢性牙周炎#
62
#牙周#
56
学习了.谢谢作者分享!
118
学习
93