Biochemia Medica:血清中钙离子浓度随时间的变化?
2019-11-03 MedSci MedSci原创
本研究的目的是比较动脉肝素化血液和静脉血清中的离子钙浓度,并研究在不同时间离心和分析的血清样品中离子钙的时间依赖性变化。
本研究的目的是比较动脉肝素化血液和静脉血清中的离子钙浓度,并研究在不同时间离心和分析的血清样品中离子钙的时间依赖性变化。
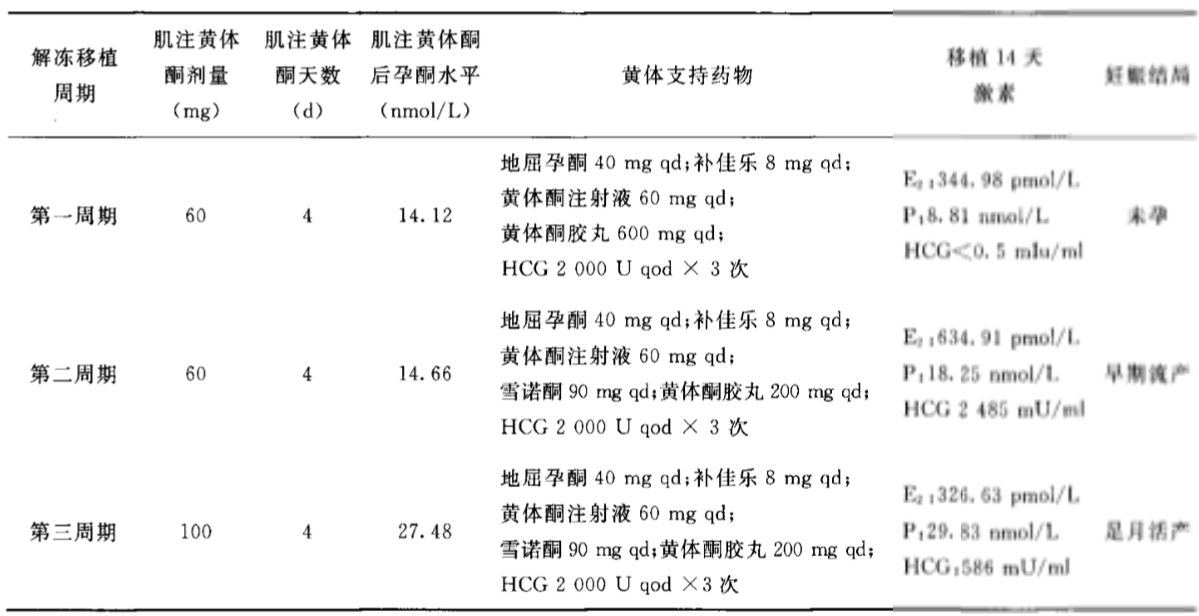
研究人员穿刺后20分钟测定动脉血中游离钙(N = 25),采样30分钟后离心10分钟测定血清中游离钙(N = 25)。在采样后15分钟,30分钟和60分钟分别离心的三支试管(N = 30)中检查了采样与离心之间的时间影响,并在10分钟内进行了分析。 在采样后30分钟离心的三支试管(N = 31)中研究了离心和分析之间的时间间隔,并进行了分析:离心后0-10、30-40和90-100分钟。 在西门子RapidLab
348EX分析仪上测量了离子钙。 使用Wilcoxon检验和ANOVA分析检验统计学意义。 根据参考变化值(RCV)判断临床意义。。
研究发现,动脉血和血清iCa值差异无统计学意义(P = 0.274)。与30分钟离心管相比,采样后60和15分钟(P = 0.005,
P = 0.003);离心30-40分钟和90-100分钟,离心0-10分钟离心管差异有统计学意义(P = 0.021,
P = 0.027)。在60与30分钟(离心),90-100与0-10和30-40分钟(分析)临床观察到明显的变化。
研究表明,及时分析动脉血样和血清血样可以交互使用。为避免临床显著差异,应在血清管采样后30min内离心,离心后30min内进行分析。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Bio#
65
#钙离子#
73
#DIC#
44
#浓度#
46
#Med#
54