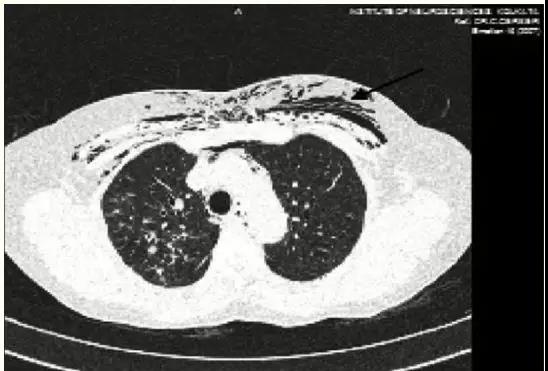
Saudi J Anaesthesia:警惕!气管插管后可能出现皮下气肿!
2019-05-08 风清扬 医博士
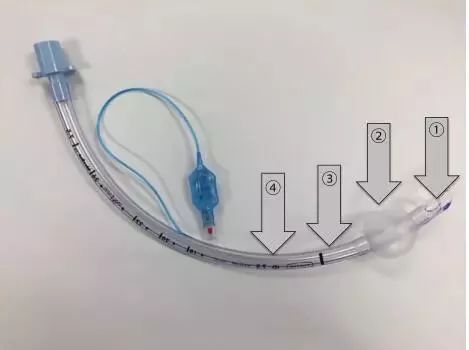
患者57岁,女性,身高150cm,50kg。全麻下接受腰椎间盘切除术。在用异丙酚和罗库溴铵诱导麻醉后,进行气管插管,较为顺利。麻醉维持采用七氟烷(FiO2=0.5)。术中未见不良事件发生,手术结束时患者可自主呼吸,取出气管插管。插管到拔管的时间为75min。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EST#
78
#ANA#
70
#皮下气肿#
80
有没有更详细解释
114
没看明白
112
#气管插管#
85
#ESI#
0