贝伐珠单抗缓解难治性卵巢颗粒细胞瘤患者的症状
2011-06-07 MedSci原创 MedSci原创
引言 近期对于贝伐珠单抗用于卵巢恶性肿瘤的研究集中在上皮恶性肿瘤中[1]。关于贝伐珠单抗用于治疗性索肿瘤,如卵巢颗粒细胞瘤的潜在作用未有评估。在此,我们报道一例难治性卵巢颗粒细胞瘤患者经贝伐珠单抗治疗后腹水症状得到缓解。 病例介绍
引言
近期对于贝伐珠单抗用于卵巢恶性肿瘤的研究集中在上皮恶性肿瘤中[1]。关于贝伐珠单抗用于治疗性索肿瘤,如卵巢颗粒细胞瘤的潜在作用未有评估。在此,我们报道一例难治性卵巢颗粒细胞瘤患者经贝伐珠单抗治疗后腹水症状得到缓解。
近期对于贝伐珠单抗用于卵巢恶性肿瘤的研究集中在上皮恶性肿瘤中[1]。关于贝伐珠单抗用于治疗性索肿瘤,如卵巢颗粒细胞瘤的潜在作用未有评估。在此,我们报道一例难治性卵巢颗粒细胞瘤患者经贝伐珠单抗治疗后腹水症状得到缓解。
病例介绍
患者为82岁老年女性,最初因“绝经后阴道出血”就诊。子宫内膜活检提示子宫内膜单纯性增生。盆腔超声发现左侧附件有一约8 × 5 × 8 cm大小的复杂性肿块。患者为进一步诊治到本研究中心。盆腔检查与超声检查一致。系统回顾发现患者除阴道出血外还有乳腺触痛。重要的实验室检查结果包括:CA125为41 U/mL;抑制素> 1000 pg/mL。子宫内膜活检病理复审确认为小灶性单纯性增生。这些结果提示疑为有激素活性的卵巢颗粒细胞瘤。
随后患者接受剖腹探查术,并进行子宫切除术,双侧附件切除(左侧卵巢囊实性肿块,盆腔及腹主动脉旁淋巴结)以及部分网膜切除术。术后恢复良好,并于第三天出院。手术病理结果为卵巢颗粒细胞瘤(IA期),局灶性单纯子宫内膜增生。组织学检查提示卵巢肿瘤细胞有极高的核分裂相,达到13/10HPF(高倍视野),流式细胞术提示存在二倍体群。肿瘤细胞中VEGF单克隆抗体免疫组化染色为强阳性(图1)。
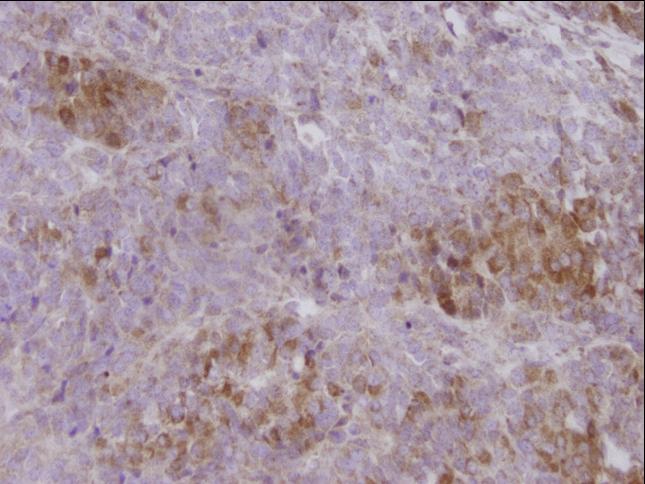
图1:卵巢颗粒细胞瘤细胞VEGF蛋白染色呈弥漫强阳性。阳性染色在细胞浆内(× 40)。
术后动态随访患者抑制素-A水平,至术后1个月时抑制素-A < 0.3 pg/mL。手术7个月后患者主诉腹胀,此时抑制素-A水平升至994.9 pg/mL。CT检查显示肿瘤扩散及腹水形成,左侧盆腔囊性病灶和毗邻脾脏处结节性病灶。患者接受BEP方案化疗,具体方案为:博莱霉素10 U d1 ~ 3,依托泊苷100 mg/m2 d1~ 3,顺铂75 mg/m2 d1,每4周一个周期。在第一周期化疗前后分别穿刺放出4.9 L和4.8 L腹水以减轻患者腹胀症状。由于博莱霉素所致的肺毒性和肾功能不全,患者化疗过程中断并在第二次化疗时将药物减量。6个周期BEP化疗方案后复查CT提示多发腹膜结节间歇性消退,腹水接近完全消退,仅在盆腔剩余少量积液。治疗后抑制素-A为3.8 pg/mL。三个月后抑制素-A再次升高至51.8 pg/mL。复查CT提示腹膜结节和腹水。此后患者又先后接受紫杉醇单药和顺铂联合依托泊苷治疗,但在治疗中患者的腹水仍持续增加,并需要反复穿刺放腹水以减轻症状,因此这2种方案均只用药2次后就未再使用。之后患者接受紫杉醇每周80 mg/m2联合贝伐珠单抗每三周15 mg/kg治疗。8次紫杉醇和3次贝伐珠单抗治疗后复查CT显示疾病稳定,仅有极少量腹水。目前患者已接受8次贝伐珠单抗联合每周一次的紫杉醇治疗。患者的抑制素-A水平也从使用贝伐珠单抗前的111.0 pg/mL降至37.9 pg/mL。目前患者不仅没有腹水相关表现、不需放腹水治疗,也没有贝伐珠单抗相关毒性的表现,并能维持体力活动,食欲和营养状态良好(白蛋白3.6 g/dL)。
讨论
肿瘤生长依赖于血管生成。血管内皮生长因子(VEGF)能有效促进血管内皮细胞分裂[2]。贝伐珠单抗是针对抗VEGF的人源化单克隆抗体。II期临床试验证实,贝伐珠单抗单药对持续、复发及顺铂耐药的卵巢癌有一定活性[3,4]。但这两项研究中纳入的患者仅为上皮来源的卵巢肿瘤和腹膜来源肿瘤。
贝伐珠单抗在复发性卵巢颗粒细胞瘤中的作用尚不清楚。在本病例中,该患者接受紫杉醇联合贝伐珠单抗的治疗,使其恶性腹水相关症状明显改善。自开始应用紫杉醇联合贝伐珠单抗后就不再需要行穿刺放腹水治疗。虽然贝伐珠单抗是与紫杉醇联合使用,而且紫杉醇对卵巢癌细胞株有明确的抗血管生成作用[5],但我们认为患者症状的改善主要是由于贝伐珠单抗的作用,因为在应用贝伐珠单抗前患者曾接受过单药紫杉醇治疗,而当时患者腹水持续存在且有明显症状。
最近的一些证据显示贝伐珠单抗可能对卵巢颗粒细胞瘤有潜在的治疗作用。Schmidt等用免疫组化法分析了32例颗粒细胞瘤肿瘤标本中VEGF的表达情况 [6],结果发现94%的颗粒细胞瘤标本中有VEGF的表达,而在10例正常卵巢对照标本中无1例表达VEGF。VEGF的阳性表达提示这些肿瘤可能对贝伐株单抗的靶向治疗敏感。
对复发性卵巢肿瘤所致恶性腹水的治疗目的是:以副反应最小的治疗获得症状控制。细胞毒药物和穿刺术都有其固有风险,并引起患者的种种不适。本病例中应用紫杉醇联合贝伐珠单抗在缓解腹水症状的同时,副反应也最小,且不再需要行穿刺术。
由于卵巢颗粒细胞瘤非常少见,因此几乎不可能设计一个随机、安慰剂对照的临床试验以评估贝伐珠单抗联合顺铂为基础的标准化疗的疗效。基于绝大多数的卵巢颗粒细胞瘤表达VEGF、贝伐珠单抗的作用机制,及本例患者经贝伐珠单抗治疗后腹水症状得到改善,我们认为贝伐珠单抗在难治性卵巢颗粒细胞瘤恶性腹水的治疗中可能有一定作用。将来还需在更多谨慎选择的难治性卵巢颗粒细胞瘤患者中进一步评价贝伐珠单抗的疗效和安全性。
参考文献
1,,Aghajanian C. The role of bevacizumab in ovarian cancer—an evolving story. Gyn Oncol 2006;102:131–3.
2,Leung DW, Cachianes G, Kuang WJ, Goeddel DV, Ferrara N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science 1989;246:1306–9.
3,Burger RA, Sill MW, Monk BJ, Greer BE, Sorosky JI. Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a Gynecologic Oncology Group study. J Clin Oncol 2007;25(33):5165–71.
4,Cannistra SA, Matulonis UA, Penson RT, Hambleton J, Dupont J,Mackey H,et al. Phase II study of bevacizumab in patients with platinum-resistant ovarian cancer or peritoneal serous cancer. J Clin Oncol 2007;25(33):5180–6.
5,Hata K, Osaki M, Dhar DK, Nakayam K, Fujiwaki R, Ito H, et al. Evaluation of the antiangiogenic effect of Taxol in a human epithelial ovarian carcinoma cell line. Cancer Chemother Pharmacol 2004;53(1):68–74.
6,Schmidt M, Kammerer U, Segerer S, Cramer A, Kohrenhagen N, Dietl J,et al. Glucose metabolism and angiogenesis in granulosa cell tumors of the ovary: Activation of M2PK, TKTL1 and VEGF. Eur J Obstet Gynecol Reprod Biol in press. [Corrected Proof. Available online 3 April, 2008].
2,Leung DW, Cachianes G, Kuang WJ, Goeddel DV, Ferrara N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science 1989;246:1306–9.
3,Burger RA, Sill MW, Monk BJ, Greer BE, Sorosky JI. Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a Gynecologic Oncology Group study. J Clin Oncol 2007;25(33):5165–71.
4,Cannistra SA, Matulonis UA, Penson RT, Hambleton J, Dupont J,Mackey H,et al. Phase II study of bevacizumab in patients with platinum-resistant ovarian cancer or peritoneal serous cancer. J Clin Oncol 2007;25(33):5180–6.
5,Hata K, Osaki M, Dhar DK, Nakayam K, Fujiwaki R, Ito H, et al. Evaluation of the antiangiogenic effect of Taxol in a human epithelial ovarian carcinoma cell line. Cancer Chemother Pharmacol 2004;53(1):68–74.
6,Schmidt M, Kammerer U, Segerer S, Cramer A, Kohrenhagen N, Dietl J,et al. Glucose metabolism and angiogenesis in granulosa cell tumors of the ovary: Activation of M2PK, TKTL1 and VEGF. Eur J Obstet Gynecol Reprod Biol in press. [Corrected Proof. Available online 3 April, 2008].
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#贝伐珠#
65
#细胞瘤#
75
#贝伐#
67
#难治性#
67
#颗粒细胞瘤#
109