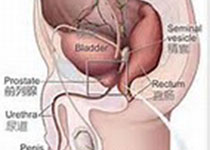
Sci Rep:膀胱癌中以可溶性Ephrin-A1 / EphA2系统为靶标,利用来氟米特对血管新生抑制作用的研究
2018-02-03 AlexYang MedSci原创
血管新生在膀胱癌中(BCa)具有重要的作用。免疫抑制药物来氟米特吸引了世界范围内的注意。然而,来氟米特在癌症中对血管新生的影响仍旧未知。最近,有研究人员报道了可溶性Ephrin-A1(sEphrin-A1)在BCa细胞系(RT4, T24和 TCCSUP)和人脐静脉内皮细胞(HUVECs)共培养上清中与永生性的泌尿上皮细胞(SV-HUC-1)和HUVECs共培养上清中相比,表达增加。sEphrin
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血管新生#
108
#抑制作用#
49
学习一下谢谢
64
#靶标#
50