教你看透——乙肝两对半结果 建议保存随时用得上!
2016-10-28 医学之声整理 医学之声整理
一、乙肝病毒检测意义: 1、HBs-Ag:乙肝表面抗原 阴性:阳性为HBV早期感染和持续感染的指标,也可能系无症状的HBV携带者。 2、HBs-Ab :乙肝表面抗体 阴性:是上述表面抗原的抗体。出现(HBs-Ab)表明机体对(HBV)产生免疫。可出现于乙肝恢复期或者注射乙肝疫苗后,也可通过输血等途径被动获得。 3、HBe-Ag:乙肝病毒e抗原 阴性:在HBs-Ag呈阳性后不久即可出现,
一、乙肝病毒检测意义:
1、HBs-Ag:乙肝表面抗原 阴性:阳性为HBV早期感染和持续感染的指标,也可能系无症状的HBV携带者。
2、HBs-Ab :乙肝表面抗体 阴性:是上述表面抗原的抗体。出现(HBs-Ab)表明机体对(HBV)产生免疫。可出现于乙肝恢复期或者注射乙肝疫苗后,也可通过输血等途径被动获得。
3、HBe-Ag:乙肝病毒e抗原 阴性:在HBs-Ag呈阳性后不久即可出现,是急性活动性感染的早期指标,在感染的高峰出现。携带者如检出HBs-Ag,表明其有较高传染性。
4、HBe-Ab:乙肝病毒e抗体 阴性:是上述e抗原的抗体。急性期从患者出现e抗原到产生e抗体的转变,证明病情好转,感染消失;携带者如检出HBc-Ab,表示其传染性低。
5、HBc-Ab:乙肝病毒核心抗体 阴性:是针对乙肝病毒核心抗原的抗体。HBc-IgM抗体:在乙肝急性期可检出高滴度的HBc-IgM,是鉴别过去感染和现在感染的指标。
二、乙肝两对半的知识
乙肝病毒(HBV)标志物有三对,由于技术方面的原因,核心抗原无法测出,便成了两对半,两对半的阳性与否仅反映是否感染了HBV和病毒复制状态,而不能反映炎症状况,与病情轻重无因果关系。
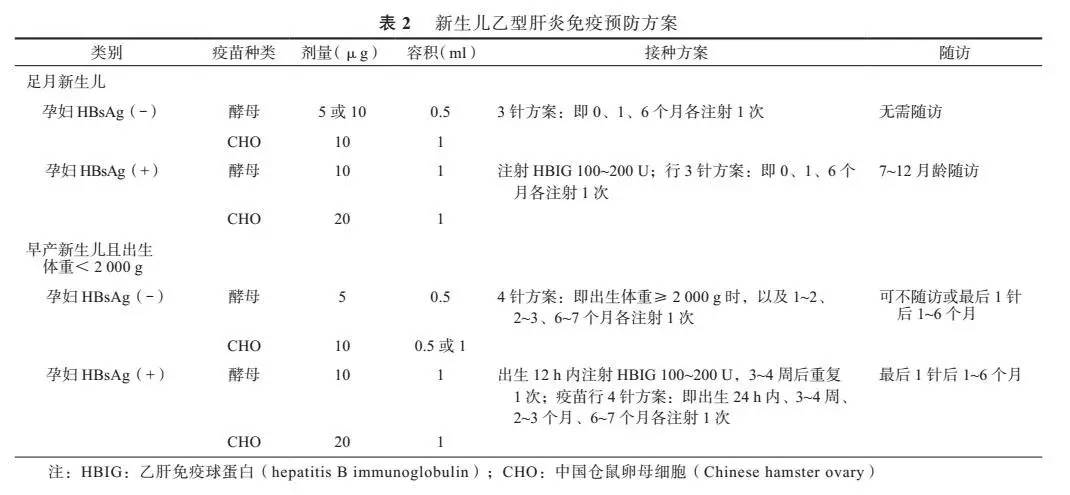
为叙述方便,今将两对半中的项目进行编号,(一般报告单顺序也是这样的)将其最常见的组合模式释疑如下:
一、乙肝表面抗原(HBsAg)
二、表面抗体(HBsAb)
三、e-抗原(HBeAg)
四、e-抗体(HBeAb)
五、核心抗体(HBcAb)
1 、一至五全部阴性:未感染过,属正常状态。可注射乙肝疫苗,以获得被动免疫。
2 、一五阳(小二阳):为急性乙肝恢复期或既往感染过,传染性较弱。①若临床无症状,ALT等肝功正常,则为无症状携带者;②有症状,ALT等明显增高,为急性乙肝早期;③有症状,ALT等正常,为慢乙肝。
3 、一三五阳(大三阳):为急慢性乙肝,提示病毒复制活跃,传染性较强。
4 、一四五阳(小三阳):为急性感染趋向恢复或慢乙肝,病毒复制不强,传染性较弱,但需检测DNA。
5 、单二阳:感染过乙肝或者注射过疫苗,现已具有免疫力,滴度越高,保护力越强,免疫时间越长。
6 、单一阳:①乙肝感染早期,病毒复制,有传染性,②若持续六个月以上阳性,为慢性乙肝病毒携带者,若滴度低小于1:16,则无传染性。
7 、单五阳:①低滴度,又IgG阳性,既往感染过,现已康复,为“带毒者”,无传染性;②若高滴度,又IgM阳性:为现时感染,是病毒复制持续的标志,有传染性,不能献血;③IgG、IgM均阳性,易发展为慢乙肝或病毒携带者。
8 、二四阳、二五阳或二四五阳:感染后康复期,已产生抗体,开始有一定的免疫力。
9 、四五阳:①为恢复期或近期感染,有低度复制与弱传染性;②病毒量少,其它标志物不易测到;③检查误差,可三个月后复查。
10 、一三阳:急性感染早期,有极强感染性。
11 、一二阳:(亚临床下同);阳性说明有病毒复制;小于等于10的五次方,传染性较低;大于等于10七次方传染性较大。文献报道,两对半五项全部阴性者仍有20%的人HBV-DNA可查到阳性,也可确诊为乙肝。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#乙肝两对半#
70
留下备用
107
谢谢分享。
109
挺好的,涨知识了……
107
总结的非常不错!收藏了
109
学习必备!号
102
这个不错,学习了
74
?
0
这个其实很基础…
75
谢谢。受益匪浅。
57