2013中国心衰指南的更新思路与要点
2013-07-10 MedSci MedSci原创
4月12日,在第15届中国南方国际心血管病学术会议上,南京医科大学第一附属医院黄峻教授介绍了我国正在修订的2013年成人心力衰竭指南(的主要框架、内容和特点以及更新修改的要点等。 黄峻教授指出,正在讨论和修订的2013版中国指南将涵盖心衰的诊断和检查、慢性心衰治疗、急性心衰治疗、心衰综合治疗和随访管理四大主题,
4月12日,在第15届中国南方国际心血管病学术会议上,南京医科大学第一附属医院黄峻教授介绍了我国正在修订的2013年成人心力衰竭指南(的主要框架、内容和特点以及更新修改的要点等。
黄峻教授指出,正在讨论和修订的2013版中国指南将涵盖心衰的诊断和检查、慢性心衰治疗、急性心衰治疗、心衰综合治疗和随访管理四大主题,并简明阐述了新指南的更新要点。
一、诊断和检查
1.积极推荐应用心衰生物学标志物BNP/NT-proBNP推荐B型利钠肽/N末端B型利钠肽前体(BNP/NT-proBNP)用于慢性心衰(Ⅱa,C),将血浆利钠肽(BNP、NT-proBNP、MR-proBNP)与心电图、二维超声心动图及多普勒超声、肌钙蛋白、X线胸片一起列为心衰常规检查。对心衰诊断尚未确定的可疑患者,可用于鉴别心源性和肺源性呼吸困难;血浆利钠肽对慢性心衰诊断敏感性和特异性较低,但可用于排除心衰诊断(BNP<100pg/ml不支持诊断)。
积极推荐BNP/NT-proBNP用于急性心衰评估。NT-proBNP<300pg/ml和BNP<100pg/ml为排除急性心衰切点;BNP/NT-proBNP对评估急性失代偿性心衰患者生存率有一定预测价值;推荐利钠肽指导治疗(急性心衰患者与基线相比,治疗后BNP/NT-proBNP下降≥30%表明治疗奏效)。
2.舒张性心衰的诊断标准主要临床表现:①典型心衰症状和体征,②左室射血分数(LVEF)正常或轻度下降(≥45%)且左心腔(尤其左室)大小正常,③相关结构性心脏病存在(如左房增大或左室肥厚)和(或)舒张功能障碍的证据,④超声心动图检查无心瓣膜疾病并可排除心包疾病、肥厚型心肌病、限制性(浸润性)心肌病等。其他需考虑因素:①符合本病的流行病学特点,如老年、病因为高血压或有高血压史、女性,部分患者伴糖尿病、房颤、肥胖或代谢综合征等;②BNP/NT-proBNP测定值轻至中度升高或至少在“灰色区域”。
二、药物和非药物治疗
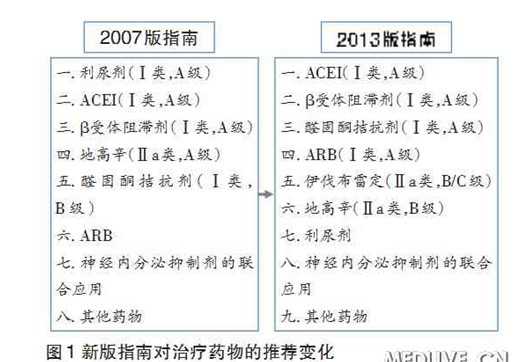
1.对治疗药物的推荐有增有改较原指南增加一类新药,即单纯降低心率的伊伐布雷定。排序方式是首先列出可改善心衰预后的药(第1~5种),继以可改善心衰症状且可长期应用的药,包括利尿剂(图1)。
2.扩大醛固酮拮抗剂应用范围适用人群从纽约心功能分级(NYHA)Ⅲ~Ⅳ级扩大至Ⅱ级,推荐等级为Ⅰa、A级证据。对应用利尿剂、血管紧张素转换酶抑制剂(ACEI)、β受体阻滞剂后疗效仍不满意的患者,推荐优先考虑加用醛固酮拮抗剂。
3.减慢心率成为慢性心衰治疗的新靶标伊伐布雷定新适应证:①已应用β受体阻滞剂、ACEI或血管紧张素受体拮抗剂(ARB)、醛固酮受体拮抗剂,仍心率≥70次/分,应该考虑使用伊伐布雷定(Ⅱa,B);②心率≥70次/分、不耐受β受体阻滞剂者,可考虑使用伊伐布雷定(Ⅱb,C)。
4.明确提出可能有害而不予推荐的药物因可能有害而明确不予推荐的药物(或组合)包括噻唑烷类降糖药、大多数钙拮抗剂(氨氯地平和非洛地平除外)、非类固醇类抗炎药和环氧合酶(COX)-2抑制剂以及在ACEI和醛固酮拮抗剂合用基础上加ARB的三药联合。因缺乏获益证据而不做推荐的药物包括能量代谢药物、肾素抑制剂、他汀、中药、鱼油等。
5.非药物治疗适应证:既扩大又加以严格限制CRT适应证扩展至适用于NYHAⅡ级患者。对药物治疗和QRS波宽度作较严格限制:窦性心律、经标准和优化抗心衰治疗至少3~6月;预期生存期>1年;如不伴左束支传导阻滞(LBBB),心功能Ⅱ级或Ⅲ~Ⅳ级患者,均要求QRS波宽度达150ms。埋藏式心律转复除颤器(ICD)被推荐用于心脏性猝死一级和二级预防。
6.ARB的用法和地位对ARB的定位:不是首先推荐药物,用于替代ACEI或在ACEI和β受体阻滞剂后仍有症状时加用;并非绝对不能与ACEI合用,但须加以限制和谨慎,因高血钾、血肌酐升高、肾功能损害等不良反应明显增多。
7.关于地高辛的临床应用(Ⅱa,B)地高辛适用于:①慢性收缩性心衰已用利尿剂、ACEI(或ARB)、β受体阻滞剂和醛固酮拮抗剂,而仍持续有症状者(主要为心功能Ⅱ~Ⅲ级者);②对伴快速心室率的房颤患者尤为适合;③对血压偏低者可考虑早期应用作为基础治疗;④已应用地高辛者不宜轻易停用。心功能NYHAⅠ级、舒张性心衰患者不宜应用。
三、治疗流程及特定情况的处理
1.有症状慢性心衰(NYHAⅡ~Ⅳ级)处理流程图(图2)
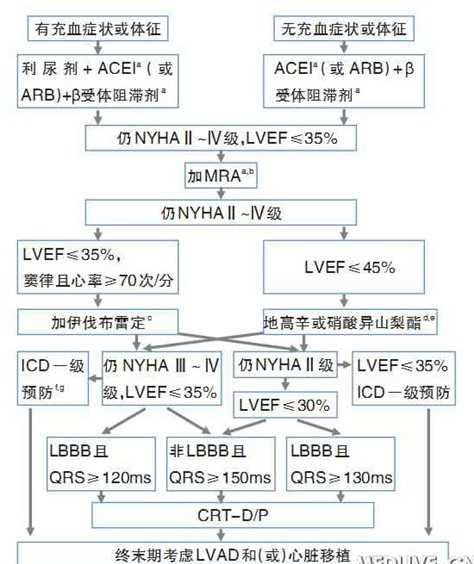
注:a、调整至有循证证据剂量或低于有循证证据剂量的最大耐受剂量。
b、如不能耐受盐皮质激素受体拮抗剂(MRA),可考虑在ACEI基础上加ARB作为替代。
c、欧洲药物管理局已批准伊伐布雷定用于心率≥75次/分者,可也考虑用于有β受体阻滞剂禁忌或不耐受者。
d、地高辛可早期用于房颤控制心室率,通常与β受体阻滞剂联用。
e、对不能耐受ACEI或ARB者可早期考虑联用肼苯哒嗪和硝酸异山梨酯。
f、对缺血性心脏病、急性心肌梗死大于40天者或非缺血性心脏病均适用。
g、NYHAIV级不是适应证。
2.舒张性心衰的治疗要点①利尿,②降压(<130/80mmHg),③控制房颤心室率,④控制心肌缺血,⑤可考虑应用β受体阻滞剂。
3.急性心衰治疗①借鉴ESC流程,去除对四肢交换加压、支气管解痉剂等的推荐;②关于急性期β受体阻滞剂应用,新增关于静脉应用方法的描述,心衰加重如与β受体阻滞剂无关则不需停用或减量,出院前宜将剂量上调;③推荐新型利尿剂托伐普坦,可用于常规利尿剂效果不佳、有低钠血症者。
4.难治性及终末期心衰治疗对经优化药物和器械治疗仍处于终末期心衰的患者,如适合心脏移植,推荐置入左室辅助装置(LVAD)或双心室辅助装置(BiVAD)(Ⅰ,B)。
5.心衰合并冠心病的处理强调基本病因为冠心病的心衰患者应接受冠脉血运重建术:对慢性心衰合并冠心病者,冠状动脉旁路移植术(CABG)适用于左主干病变(Ⅰ,C)或双支、三支病变(Ⅰ,B),患者预期寿命应>1年;经皮冠状动脉介入术(PCI)适用于上述患者、但不宜行外科手术者;无心绞痛或无存活心肌者,不宜作血运重建术。
四、综合治疗
心衰整体治疗包括运动训练和康复(Ⅰ,a)、多学科管理(Ⅰ,a)及姑息治疗。重视心衰患者随访管理,包括一般性随访(1~2个月1次)、重点随访(3~6个月1次)、动态监测[利钠肽指导治疗(Ⅱb,C)]等及患者教育。
五、其他
1.名称因更新指南内容未包括儿童,故名称将突出“成人”。
2.心衰发病机制病理生理机制部分将增加心肌损伤的表述,即在发生心肌重构的机制中,除神经内分泌系统(如肾素-血管紧张素-醛固酮系统和交感神经系统)过度激活外,提出心肌急性损伤(如急性心肌梗死、重症心肌炎所致的心肌坏死)也是一主要原因。
3.修改对限钠、限水的描述限钠对控制Ⅲ~Ⅳ级心衰患者充血症状和体征有帮助;急性心衰伴容量负荷过重者,限制钠摄入<2g/d。严重低钠血症(血钠<130mmol/L)、液体摄入量应<2L/d。对所有轻中度症状患者常规限制液体可能无益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#心衰指南#
79
#新思路#
45
good
124
good
120
舒张性心衰降压的治疗规则,药物选择
144
舒张性心衰的降压治疗可否有详细规则
155