PNAS:乳腺癌治疗的新方法“免疫激活细胞因子”
2017-12-19 白木清水译自 medicalxpress 来宝网
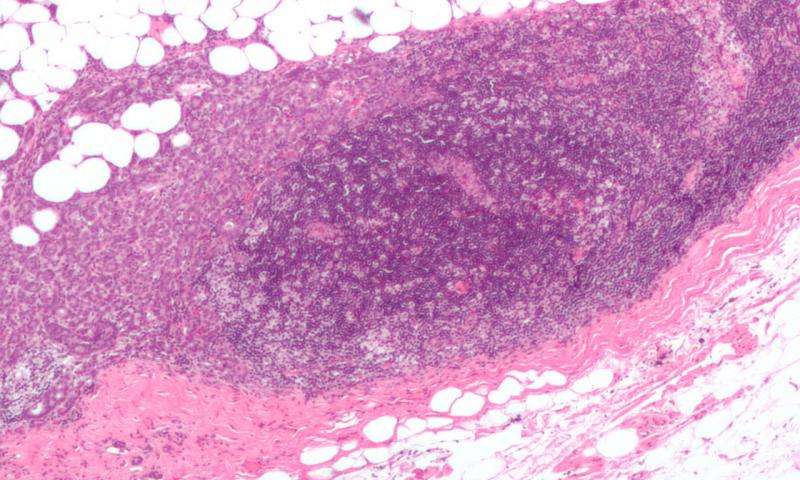
根据凯斯西储大学医学院病例综合癌症中心的最新研究,最致命的乳腺癌形式可能有新的治疗选择。在“美国国家科学院院刊”上,研究人员发现,三阴性乳腺癌细胞极易受干扰素-β一种有效的抗微生物药物的影响,这种抗微生物药物也能激活免疫系统。这项新的研究显示干扰素-β损害乳腺癌细胞迁移和形成肿瘤的能力。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胞因子#
66
#新方法#
0
#活细胞#
101
#PNAS#
61
#细胞因子#
0
三阴性乳腺癌是一种最致命.最具侵略性的乳腺癌
141