Transl Lung Cancer Res: 在EGFR突变晚期NSCLC患者使用EGFR-TKI治疗失败后,化疗-抗血管生成对比化疗-免疫治疗联合治疗的疗效
2022-02-08 yd2015 MedSci原创
研究表明,在EGFR-TKI治疗失败后,化疗-免疫联合治疗的疗效与化疗-抗血管生成联合治疗的疗效相当。对于EGFR T790M突变的患者,化疗-抗血管生成联合治疗可能是首选的治疗方案。
EGFR突变晚期NSCLC患者标准治疗为EGFR-TKI,尽管有效,但是最终难免出现耐药。对于EGFR-TKI治疗进展后,后续的最佳治疗方案尚不清楚。因此,同济大学医学院附属上海市肺科医院团队开展了真实世界研究,评估在EGFR突变晚期NSCLC患者使用EGFR-TKI治疗失败后,化疗-抗血管生成对比化疗-免疫治疗联合治疗的疗效。相关结果发表在Translational Lung Cancer Research杂志上。
我们筛查2015年1月至2020年12月期间诊断EGFR突变的晚期NSCLC患者,在EGFR-TKI耐药后,接受化疗-抗血管生成或化疗-免疫疗法联合治疗。收集患者信息,评估客观缓解率(ORR)、疾病控制率(DCR)和无进展生存期(PFS)。
共纳入144例患者,所有患者的中位年龄为61岁(范围为19-76岁),52.8%的患者为女性。所有患者病理诊断为肺腺癌。共有110例(76.4%)患者不吸烟。接受化疗-抗血管生成联合治疗的患者比例(100/ 144,69.4%)高于化疗-免疫联合治疗的患者(44/ 144,30.6%)。
144例患者中,131例(91.0%)接受EGFR- TKIs单药治疗,13例(9.0%)接受EGFR- TKIs联合其他治疗,包括抗血管生成治疗(6,4.2%)、放疗(5,3.5%)和化疗(2,1.4%)。129例(89.6%)患者接受了EGFR-TKIs作为一线治疗,14例(9.7%)患者接受了二线治疗,1例(0.7%)患者接受了三线及以上治疗。
所有患者使用EGFR-TKIs治疗的ORR和DCR分别为60.2%和93.2%,中位无进展生存期为10.42个月。EGFR-TKI耐药后,29例(20.1%)患者检测到T790M二次突变。其中23例(79.3%)患者接受了第三代EGFR-TKIs作为后续治疗。
EGFR-TKI治疗进展后,化疗-免疫联合治疗比化疗-抗血管生成联合治疗获得更高的客观缓解率(ORR) (29.5% vs. 13.0%, P=0.017),但两组间的DCR相似(93.0% vs. 88.6%, P=0.585)。化疗-免疫联合治疗组中位PFS略长,但无统计学意义(7.59 vs. 6.90个月,P=0.552, HR =0.875, 95% CI: 0.565 1.355)。总生存期(OS)在数据截止时尚未成熟。

在亚组分析中,接受化疗-抗血管生成联合治疗的19del和L858R突变患者的ORR和PFS无显著差异(ORR: 10.9% vs. 11.8%, P=1.000;中位PFS: 7.74 vs. 7.30个月,P=0.702, HR =0.920, 95% CI: 0.594 1.426)。此外,T790m阳性和T790m阴性患者在TKI耐药后的ORR和PFS类似(ORR: 9.5% vs. 13.2%, P=0.942;中位PFS: 5.33 vs. 7.46个月,P=0.202, HR =1.459, 95% CI: 0.737-2.890)。

对于接受免疫化疗联合治疗的患者,EGFR L858R突变组的ORR和PFS优于19del突变组,但无显著差异(ORR: 33.3% vs. 22.7%, P=0.438;中位PFS: 7.59 vs. 5.65个月,P=0.798, HR =0.899, 95% CI: 0.392-2.059)。
然而,在EGFR- TKI治疗后发生继发性T790M突变的患者更不可能从化疗-免疫治疗联合获益(ORR: 14.3% vs. 32.4%, P=0.608;中位PFS: 3.42 vs. 7.63个月,P=0.028, HR =3.028, 95% CI: 0.575-15.94)。
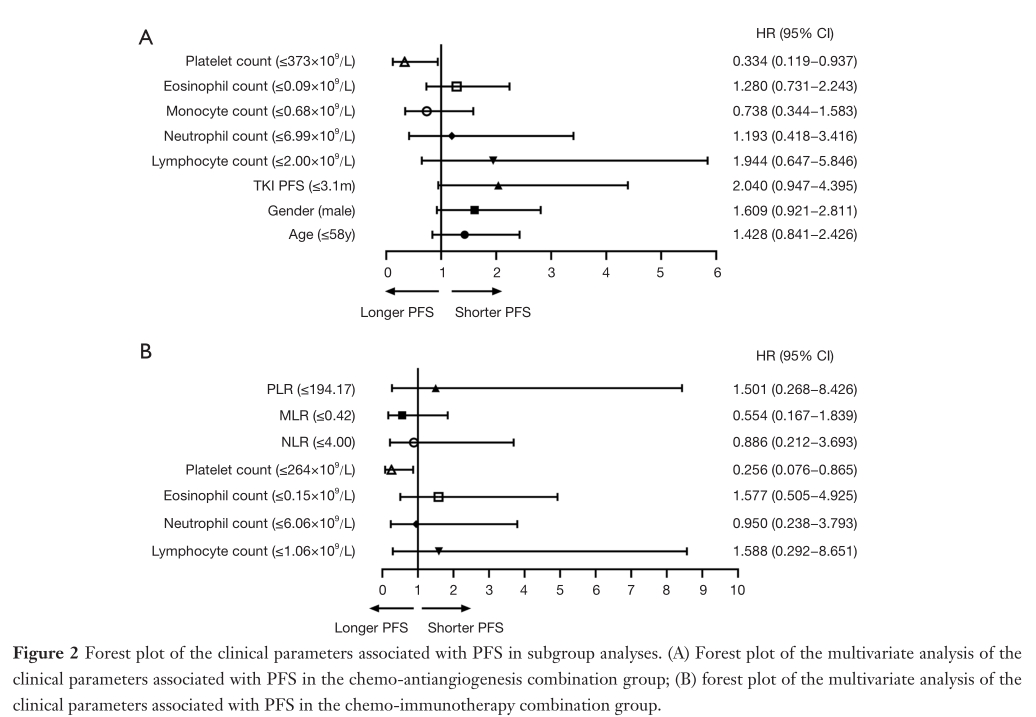
多因素分析显示,在化疗-抗血管生成联合治疗组中,仅有血小板计数≦373 10 9 /L与PFS延长独立相关(P=0.037, HR =0.334, 95% CI: 0.119 0.937)。在化疗-免疫联合治疗组中,血小板计数≦264 10 9 /L与PFS延长独立相关(P=0.028, HR =0.256, 95% CI: 0.076 0.865)。


综上,研究表明,在EGFR-TKI治疗失败后,化疗-免疫联合治疗的疗效与化疗-抗血管生成联合治疗的疗效相当。对于EGFR T790M突变的患者,化疗-抗血管生成联合治疗可能是首选的治疗方案。此外,血小板计数可能是EGFR-TKI治疗失败后患者的潜在预后因素。
原始出处:
Yu X, Li J, Ye L, Zhao J, Xie M, Zhou J, Shen Y, Zhou F, Wu Y, Han C, Qian J, Chu T, Su C. Real-world outcomes of chemo-antiangiogenesis versus chemo-immunotherapy combinations in EGFR-mutant advanced non-small cell lung cancer patients after failure of EGFR-TKI therapy. Transl Lung Cancer Res 2021;10(9):3782-3792. doi: 10.21037/tlcr-21-681
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Transl#
101
#治疗失败#
81
#抗血管#
98
#TRA#
60
#SCLC患者#
92
#联合治疗#
73
#EGFR-TKI#
104
#TKI#
75
#NSCLC患者#
67
#晚期NSCLC#
73