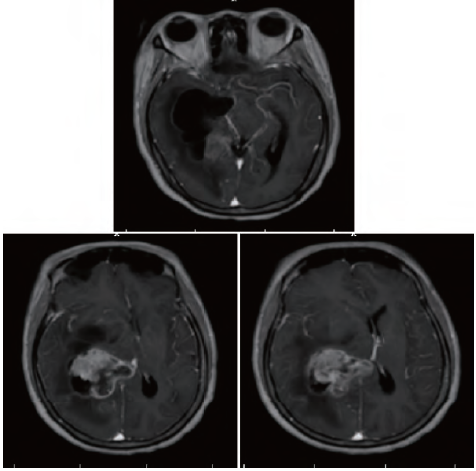
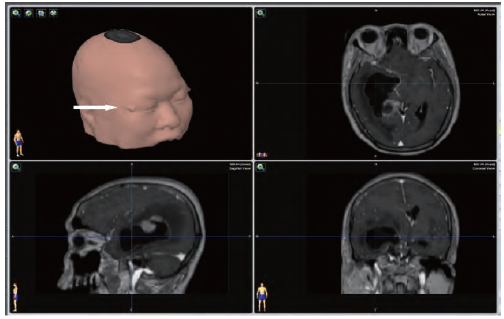
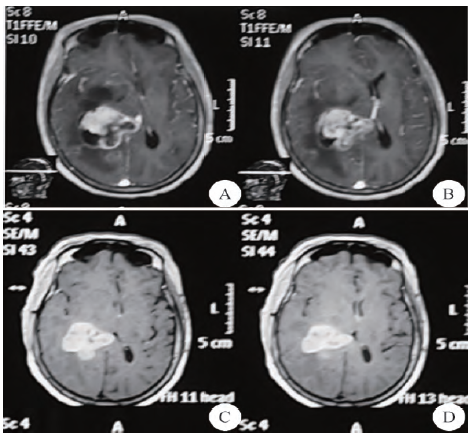
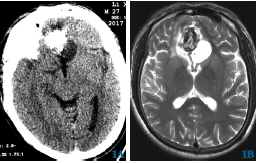
脑室外引流术联合分次立体定向放射外科治疗巨大脑转移瘤
2019-07-23 甄俊杰 洪伟平 王辉 临床神经外科杂志
患者女性,59岁。因“右上肺癌综合治疗后9个月,头痛2周,加重2d”于2013年9月15日急诊入院。患者于2012年12月因“左髋部疼痛2个月”在某三甲医院就诊,行CT引导下经皮肺穿刺活检,病理示:中分化鳞癌,EGFR突变检测:21外显子突变。诊断为:右上肺中分化鳞癌T1N1M1(左髂骨),Ⅳ期。给予吉非替尼治疗,剂量为250mg,每日一次,口服。并行左髂骨姑息止痛放疗,剂量30Gy/10F,3G
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#脑室外引流#
116
#定向#
73
#转移瘤#
75
#立体定向#
76
#脑转移瘤#
83
#脑室#
0