Cell Host & Microbe :抗生素可能恶化哮喘症状
2014-01-17 佚名 生物360
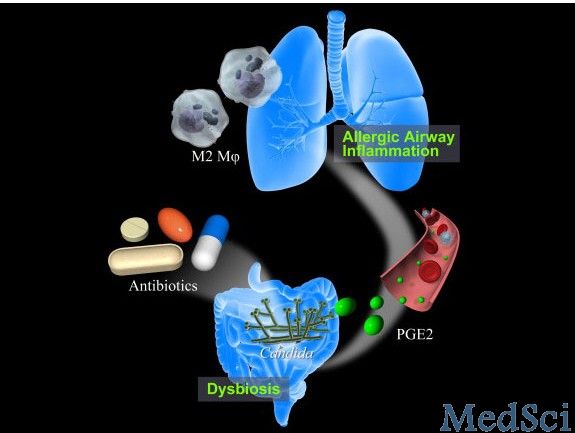
日前,日本筑波大学的研究人员发现,服用抗生素会破坏实验鼠肠道的菌群平衡,从而使哮喘症状恶化。相关论文在线刊登在了近期的《细胞-宿主与微生物》Cell Host & Microbe杂志上。研究中,科学家让实验鼠吸入会导致过敏的物质,使其患上哮喘。结果显示,如果实验鼠预先服用了抗生素,其哮喘症状比未服用抗生素的实验鼠更严重,支气管内引发炎症的细胞数量相当于后者的约 2 倍。研究人员发现,在服用
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CRO#
51
#Cell#
54
#CEL#
55
#Micro#
50