Gastrointest Endosc:内镜治疗肠化生完全缓解后复发率高
2016-06-06 高晓方 翻译 中国医学论坛报
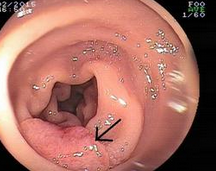
美国一项研究表明,内镜治疗肠化生完全缓解(CRIM)后复发率高,因此,CRIM后的持续监测很有必要。论文发表于《消化内镜》杂志6月刊[Gastrointest Endosc2016,83(6):1090]。 该研究检索多个数据库中内镜治疗CRIM后的长期随访研究,估算CRIM后复发性肠化生、不典型增生Barrett食管和高度不典型增生(HGD)或食管腺癌(EAC)每人-年随访的汇总发病率,评估
美国一项研究表明,内镜治疗肠化生完全缓解(CRIM)后复发率高,因此,CRIM后的持续监测很有必要。论文发表于《消化内镜》杂志6月刊[Gastrointest Endosc 2016,83(6):1090]。
该研究检索多个数据库中内镜治疗CRIM后的长期随访研究,估算CRIM后复发性肠化生、不典型增生Barrett食管和高度不典型增生(HGD)或食管腺癌(EAC)每人-年随访的汇总发病率,评估与复发相关的因素。
结果显示,41项研究的4443例患者符合入选标准,随访超过10427人-年,复发患者为795例。所有内镜治疗模式,复发性肠化生、不典型增生Barrett食管和HGD或EAC每人-年的汇总发病率分别为7.1%、1.3%和0.8%。患者年龄的增加和Barrett食管的病变长度可预测肠化生复发;内镜治疗后复发率为97%。
原始出处:
Krishnamoorthi R1, Singh S1, Ragunathan K2, A Katzka D1, K Wang K1, G Iyer P1.Risk of recurrence of Barrett's esophagus after successful endoscopic therapy.Gastrointest Endosc. 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#GAS#
50
#Test#
57
#完全缓解#
59
#EST#
51
#AST#
51
#复发率#
49
#内镜#
0
#内镜治疗#
55
#肠化生#
56