Cell:抑制TAK1蛋白促进结肠癌细胞凋亡
2012-04-10 Beyond 生物谷
近日,美国波士顿大学医学院药理学和实验疗法部助理教授Anurag Singh博士在芝加哥召开的美国癌症研究届年会上公布了他最近有关靶向治疗结肠癌的工作进展。相关研究论文发表在Cell杂志上。 每年,有超过一百万的结肠癌病例被确诊,在全世界范围内结肠癌会造成约60万人死亡。这些病例中有一半以上发现有KRAS基因的突变。在美国,结肠癌患者的KRAS基因突变是非常常见的,但靶向KRAS基因的治疗药物临

近日,美国波士顿大学医学院药理学和实验疗法部助理教授Anurag Singh博士在芝加哥召开的美国癌症研究届年会上公布了他最近有关靶向治疗结肠癌的工作进展。相关研究论文发表在Cell杂志上。
每年,有超过一百万的结肠癌病例被确诊,在全世界范围内结肠癌会造成约60万人死亡。这些病例中有一半以上发现有KRAS基因的突变。在美国,结肠癌患者的KRAS基因突变是非常常见的,但靶向KRAS基因的治疗药物临床效益却不甚乐观。因此,KRAS基因突变的患者通常都面临非常有限的治疗选择,并且临床预后很差。
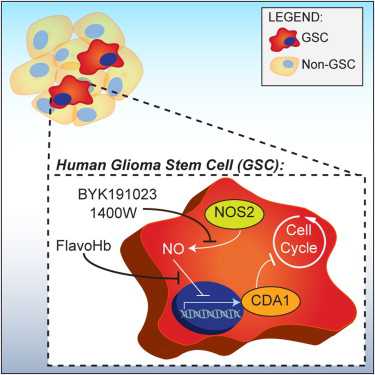
Singh和他的同事们已经确定了KRAS基因突变的结肠癌中处于过度激活的一些基因。其中包括MAP3K7或TAK1蛋白基因,这两蛋白在促进结肠癌病情恶化中起着非常关键的作用。抑制TAK1蛋白的结果是杀死KRAS基因突变的肿瘤细胞,但对正常非突变的细胞影响很小。Singh说:抗TAK1的蛋白拮抗剂可能为侵略性的KRAS基因突变的结肠癌患者提供“个性化”中医学治疗。研究人员目前正努力测试TAK1蛋白抑制剂的临床疗效。(生物谷:Bioon)

doi:10.1016/j.cell.2011.12.033
PMC:
PMID:
TAK1 Inhibition Promotes Apoptosis in KRAS-Dependent Colon Cancers
Anurag Singh, Michael F. Sweeney, Min Yu, Alexa Burger, Patricia Greninger, Cyril Benes, Daniel A. Haber, Jeff Settleman
Colon cancers frequently harbor KRAS mutations, yet only a subset of KRAS mutant colon cancer cell lines are dependent upon KRAS signaling for survival. In a screen for kinases that promote survival of KRAS-dependent colon cancer cells, we found that the TAK1 kinase (MAP3K7) is required for tumor cell viability. The induction of apoptosis by RNAi-mediated depletion or pharmacologic inhibition of TAK1 is linked to its suppression of hyperactivated Wnt signaling, evident in both endogenous and genetically reconstituted cells. In APC mutant/KRAS-dependent cells, KRAS stimulates BMP-7 secretion and BMP signaling, leading to TAK1 activation and enhancement of Wnt-dependent transcription. An in vitro-derived TAK1 dependency signature is enriched in primary human colon cancers with mutations in both APC and KRAS, suggesting potential clinical utility in stratifying patient populations. Together, these findings identify TAK1 inhibition as a potential therapeutic strategy for a treatment-refractory subset of colon cancers exhibiting aberrant KRAS and Wnt pathway activation.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
84
#Cell#
71
#癌细胞#
57
#细胞凋亡#
49