J Thromb Haemost:他汀类药物可以降低复发性静脉血栓形成风险
2016-10-05 Mechront 译 MedSci原创
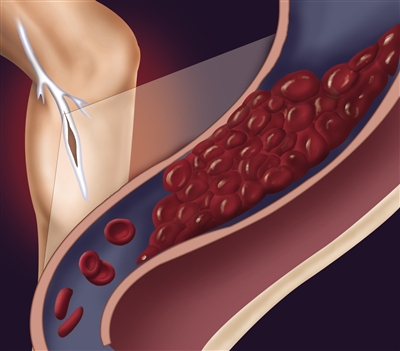
根据一项以人群为基础的队列研究的结果,对于既往发生过静脉血栓形成的患者,使用他汀类药物可以降低复发性静脉血栓形成的风险。 华盛顿大学流行病学系教授Nicholas L. Smith博士称:虽然抗凝治疗可有效的预防血栓复发,但长期治疗存在大出血风险。如果能寻找到既不增加出血风险,又可以降低复发风险的替代方法就是提高临床管理的关键。 因此他们进行了研究,评估他汀类药物能否降低复发性静脉血栓
根据一项以人群为基础的队列研究的结果,对于既往发生过静脉血栓形成的患者,使用他汀类药物可以降低复发性静脉血栓形成的风险。
华盛顿大学流行病学系教授Nicholas L. Smith博士称:虽然抗凝治疗可有效的预防血栓复发,但长期治疗存在大出血风险。如果能寻找到既不增加出血风险,又可以降低复发风险的替代方法就是提高临床管理的关键。
因此他们进行了研究,评估他汀类药物能否降低复发性静脉血栓形成的风险。
研究纳入了2798名(平均年龄为65.8岁,55%为女性)经历了静脉血栓形成(53%肺栓塞)的患者,在这些患者中,204例(7.3%)患者在静脉血栓形成事件的30天内死亡。
在基线时,22.1%的患者接受降脂治疗(98.7%为他汀类药物),24%的患者存在心血管疾病。
中位随访时间为3.4年(范围0-11)。在这段时间内,16%(n = 457)的患者经历了复发性静脉血栓形成;这类复发者中39%的为肺栓塞。7%的患者出现心血管疾病,21%的患者开始他汀类药物治疗。在基线时使用他汀类药物治疗的患者中,,27%的患者在随访过程中停止治疗;总的来说,38%的患者在随访过程中使用他汀类药物。
使用他汀类药物患者的静脉血栓复发率为5.2/100人年 (95% CI, 4.7-5.9);目前服用他汀类药物患者的静脉血栓复发率为3.9/100人年 (95% CI, 3.3-4.7)。
目前使用他汀类药物治疗可以降低复发性静脉血栓形成的风险(HR = 0.74; 95% CI, 0.59-0.94)。对随访过程中才开始使用他汀类药物的患者(HR = 0.62; 95% CI, 0.41-0.93)或没有心血管疾病的患者(HR = 0.62; 95% CI, 0.45-0.85)进行分析,仍然得到类似结论。
他汀类药物降低静脉血栓形成的复发风险这方面,最显著的是辛伐他汀(HR = 0.76; 95% CI, 0.57-1)。
研究人员承认,非随机性的他汀类药物的使用数据可能混淆分析结果。
原始出处:
Statin use linked to decreased risk for recurrent venous thrombosis.helaio.October 4, 2016
Smith NL, et al. The association of statin therapy with the risk of recurrent venous thrombosis.J Thromb Haemost. 2016;doi:10.1111/jth.13334.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#复发性#
81
#降低复发#
62
#HAE#
60
#他汀类药#
81
#静脉#
78
#静脉血#
46
好文章,可以应用
128
继续关注!
132
谢谢分享!
126
好文章,受益
98