JACC:HDL-P与颈动脉粥样硬化进展独立相关
2015-02-04 伊文 心在线
首都医科大学附属北京安贞医院-北京市心肺血管疾病研究所齐玥、赵冬等的一项队列分析研究,首次报道了高密度脂蛋白颗粒(HDL-P)胆固醇过载(cholesterol-overloaded)与颈动脉粥样硬化密切相关。该结果发表于《美国心脏病学会杂志》[J Am Coll Cardiol. 2015; 65(4):355-63]。 该研究共纳入930例45~75岁受试者,按照高密度脂蛋白(HDL
首都医科大学附属北京安贞医院-北京市心肺血管疾病研究所齐玥、赵冬等的一项队列分析研究,首次报道了高密度脂蛋白颗粒(HDL-P)胆固醇过载(cholesterol-overloaded)与颈动脉粥样硬化密切相关。该结果发表于《美国心脏病学会杂志》[J Am Coll Cardiol. 2015; 65(4):355-63]。
该研究共纳入930例45~75岁受试者,按照高密度脂蛋白(HDL)胆固醇(HDL-C)与HDL-P数量比值(HDL-C/P)分组。
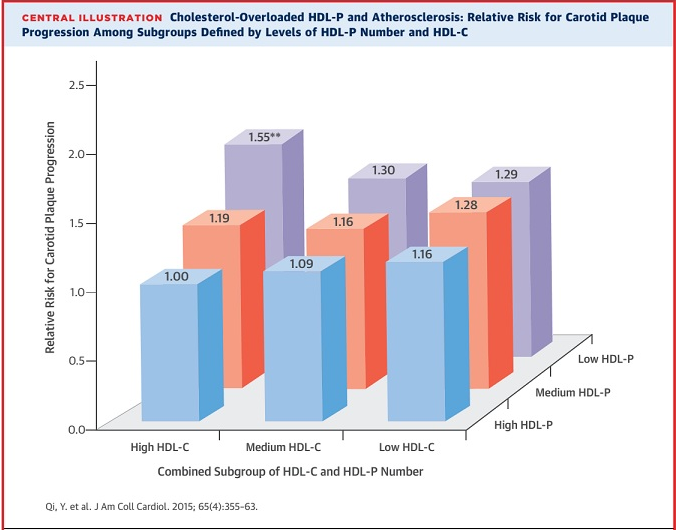

随访5年发现,基线HDL-C/P与颈动脉粥样硬化进展显著相关。其中,HDL-C/P最高组受试者的颈动脉粥样硬化进展速度是最低组的1.56倍。此外,在基线时没有斑块的受试者中,HDL-C/P最高组受试者的总斑块面积(TPA)比最低组大9.4 mm2。
研究者认为,HDL-P数量及胆固醇含量联合决定了HDL的抗动脉粥样硬化功能。HDL-P胆固醇过载与动脉粥样硬化风险正相关,这也许能解释,为何部分临床研究中血浆HDL-C水平升高后受试者未能获益。
原始出处:本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








值得珍藏!
136
#JACC#
79
#粥样硬化#
61
#颈动脉#
60
已阅
138
明白
133
#HDL#
57
#ACC#
54
#颈动脉粥样硬化#
64