病例信息
基本信息:52岁,女性,右肺占位一周。
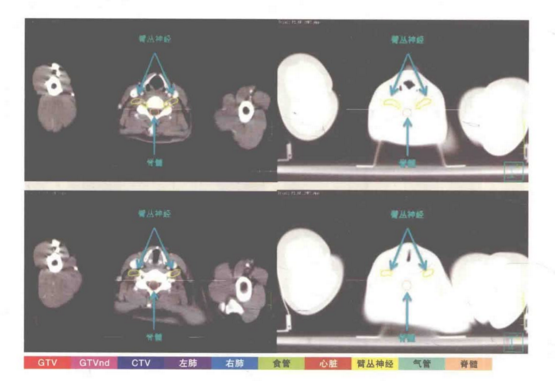
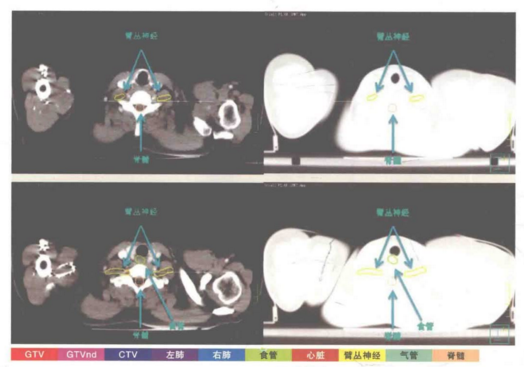
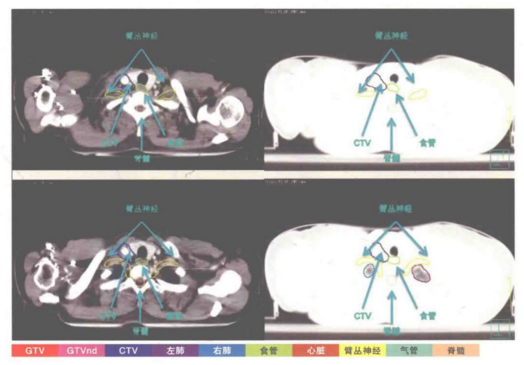
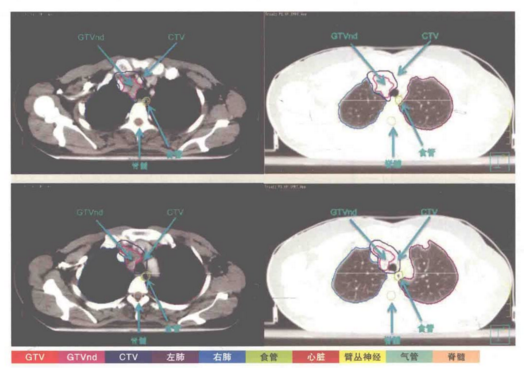
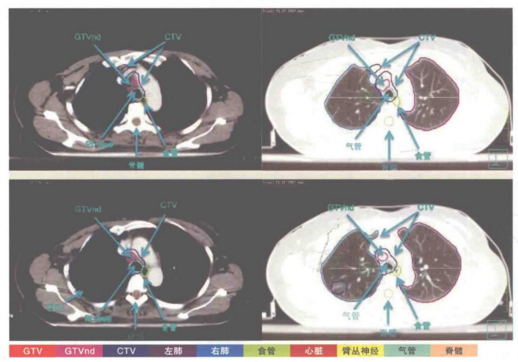
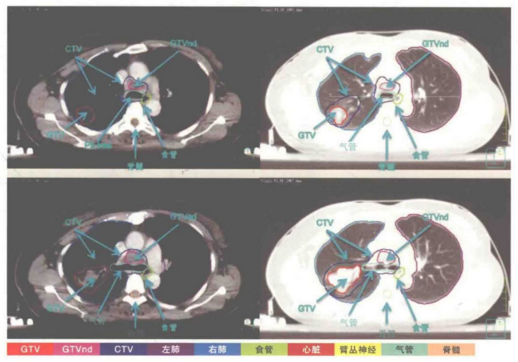
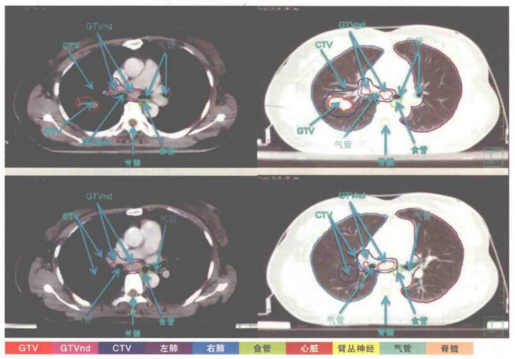
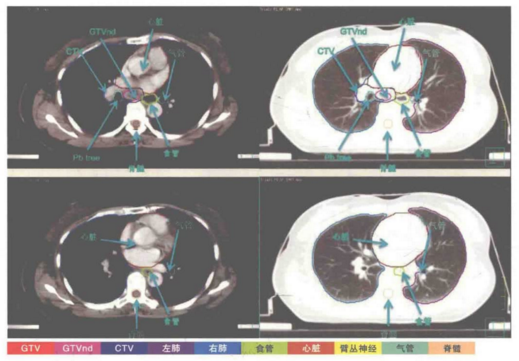
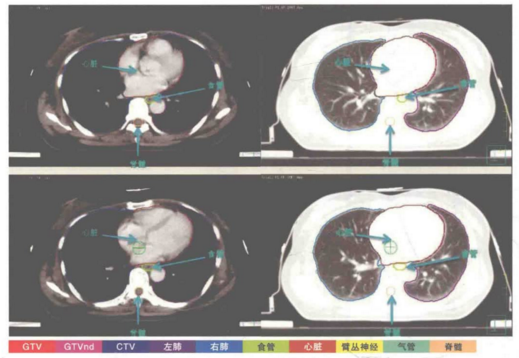
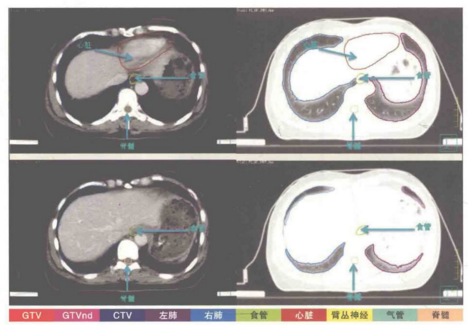
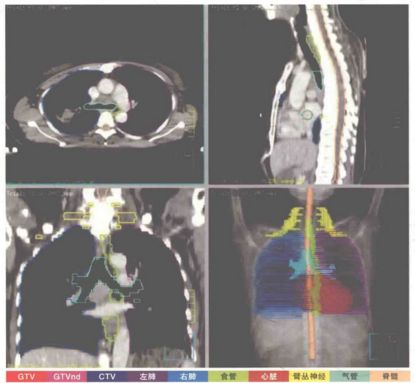
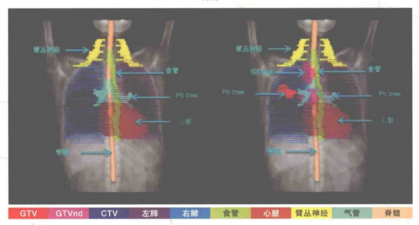
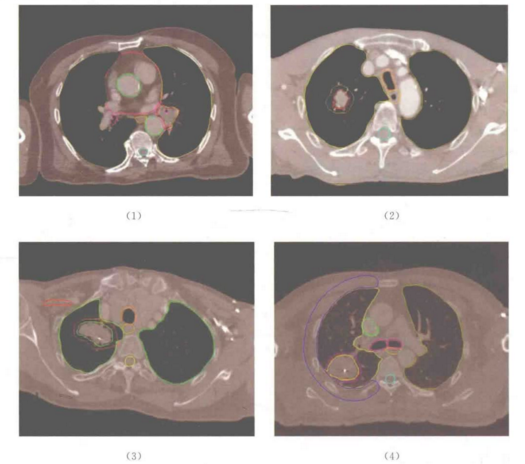
诊断:右肺上叶低分化腺癌ⅢA期。
治疗经过:PET-CT示:右肺上叶后段不规则肿物,4.3cm✖2.5cm,伴代谢增高,右肺门及纵横(2R、3A、4R、7区)多发肿大淋巴结伴代谢增加,考虑转移。支气管镜活检病理:低分化腺癌。
免疫组化:CK18(3+),TTF1(3+),CK5/6(-)EGFR(2+)。放疗靶区:右侧上叶肿物,右肺门,纵隔2R、3A、4R、7区淋巴结引流区。体位:仰卧位热塑体膜固定,双手保肘置于额前,体表标记:体中线第7胸椎水平。




参考文献:
[1]袁双虎,宋启斌主编.肿瘤精准放疗靶区勾画图谱[M].武汉:湖北科学技术出版社.2018.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#靶区#
72
#非小细胞#
62
#局部晚期#
82
#靶区勾画#
69
#局部#
67
学习
98