Cell:血管紧张素受体——瞄准人类健康的隐形杀手
2015-04-28 佚名 生物通
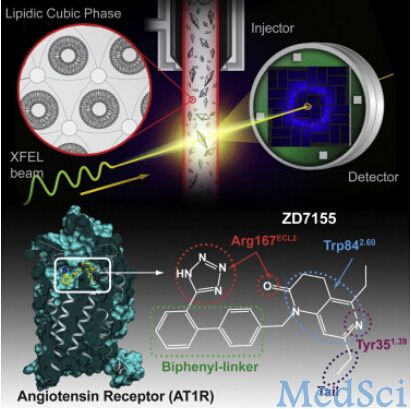
每三个美国人中就有一人罹患高血压,这一人类健康的隐形杀手可以导致冠心病、心力衰竭和中风等疾病。利用一种先进的X-射线分析技术,由来自美国、德国的科学家组成的一个研究小组,揭示出了人体中最重要的血压调控因子——血管紧张素受体AT1R的分子结构。他们的研究结果发表在4月23日的《细胞》(Cell)杂志上。南加州大学Dornsife文理学院首席研究员及教授Vadim Cherezov说,这项研究工作有可
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#人类健康#
67
#CEL#
55
#Cell#
61
相关研究应该了解
161
#血管紧张素#
61