病例简介
77岁男性患者,因“间断心前区疼痛3天余,加重4小时”就诊。
查体:神清,血压135/ 85 mmHg,双肺呼吸音粗,未闻及干湿啰音,心率66次/分,律齐,各瓣膜听诊区未闻及病理性杂音及心包摩擦音。否认吸烟饮酒史。
急诊心肌损伤标志物:Myo 28.7 ng/ml,cTnI<0.05 ng/ml,CKMB:1.5 ng/ml,NT-proBNP 200 pg/ml;
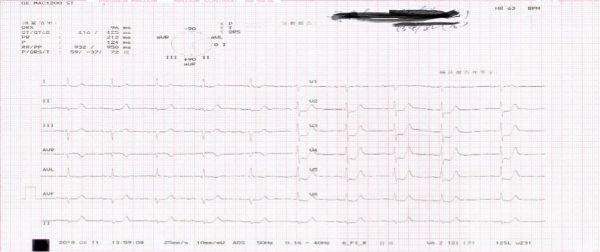
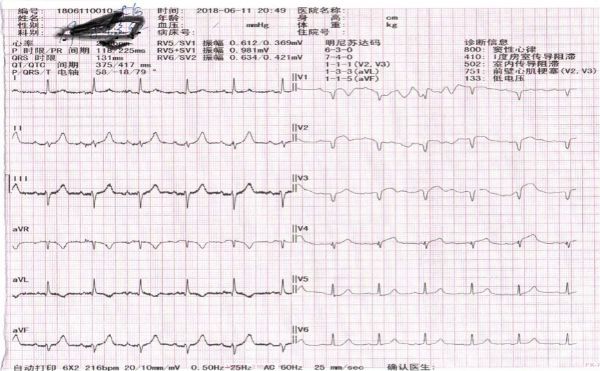
急诊心电图:
先后给予扩冠、抗血小板,吸氧等治疗,患者仍有胸痛发作,急查胸痛三联CT,未见主动脉夹层及肺栓塞。因怀疑急性冠脉综合征,行急诊冠脉造影检查,结果示LM未见明显狭窄,LAD自近段完全闭塞,LCX近段可见70%狭窄,OM1开口85%狭窄;RCA近段至远段弥漫病变,最重处60%狭窄,后侧枝远段80%狭窄。考虑LAD为罪犯病变,遂于LAD病变处置入两枚支架。
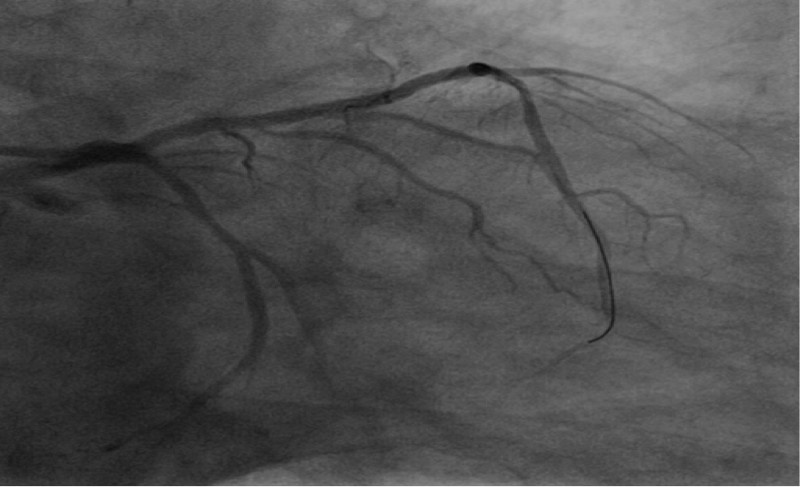
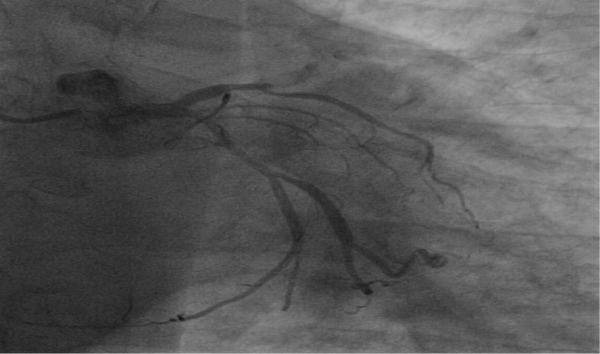
术前造影
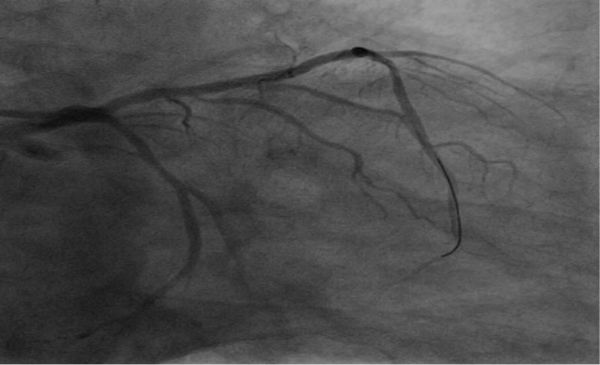
术后造影
术后心电图
患者术后胸痛缓解,继续给予双联抗血小板、稳定斑块、扩冠、抗凝等处理,术后一周患者康复出院。
讨论分析
LAD急性闭塞的心电图常表现为胸前导联ST段弓背向上抬高,容易辨识,提示医生及时行冠状动脉再灌注治疗。而De Winter综合征是新近提出的定义,其心电图胸前导联ST段不抬高,而呈上斜性压低,往往提示LAD急性闭塞,需要急诊再灌注治疗。
2008年De Winter等发现在1532例前壁心肌梗死的患者中,有30例患者出现特征性的心电图改变,约占2%。并认为心电图自始至终也不会出现胸前对应导联的ST 段抬高或动态变化,而且造影均未发现LM病变,罪犯血管多为LAD近段,多通过急诊PCI 治疗后心电图回归正常。
其主要心电图特征表现为:①胸前导联T 波导联高尖对称;②V1-V6导联的ST 段在J点后上斜型压低1-3mm;③QRS波群通常不增宽或轻微增宽;④可出现胸前导联R 波递增不良;⑤大多数患者avR导联ST段抬高1-2 mm。
De Winter ST-T改变(即V1-V6 导联ST段上斜型压低)往往提示了LAD 近段完全闭塞或者次全闭塞(也有高位对角支闭塞出现),病情通常比较危重,应当把心电图上这种改变作为STEMI的等危症进行管理。而De Winter综合征心电图改变的电生理机制仍不明确,可能与蒲肯野纤维的解剖变异导致心内膜传导延迟有关。另外,ST 段不抬高也可能与细胞膜上ATP敏感性钾通道不能激活有关,其机制是心肌缺血使ATP产生缺乏。
本例胸痛患者心电图改变与De Winter ST-T改变完全符合。本文通过具体实例,使读者能够重视并识别高危ACS患者心电图的不典型变化,使广大临床医生对De Winter 综合征的心电图有更深层次地理解,对临床工作有很大的启迪借鉴作用。
作者简介
作者:赵凯,祁建丽,李永健
作者单位:天津市中西医结合医院(南开大学附属南开医院)心内一科
作者简介:赵凯,南开大学附属南开医院心内一科副主任医师,天津市131创新型人才“第一层次”人选,国家自然科学基金委员会项目评审专家,北京医学会心血管病学分会京津冀CTO介入治疗俱乐部委员,天津市健康教育巡讲专家以及多家SCI杂志审稿人。曾获天津市“南开区十大杰出青年”提名奖,GW-ICC长城青年医师奖,天津市科技成果奖,CSC/OCC“青年优秀论文英语演讲比赛三等奖”。
原始出处:
[1] 徐萌萌, 姜龙, 冯娜娜, 等. De Winter 综合征一例. 中华心血管病杂志, 2018,46(3): 230-231.
[2] de Winter RJ,Verouden NJ, Wellens HJ, et al. A new ECG sign of proximal LAD occlusion. NEngl J Med, 2008, 359(19): 2071-2073.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ACS#
55
#漏诊#
58
学习了新知识.
84
好文献学习了
71
了解了解.学习学习
81
好好好好好好好好
106